Procedure associated with reduced risks and high curative rates

Although the incidence of gastric and esophageal cancers in the United States has decreased slightly during the past decade, these two cancers still represent a significant portion of upper gastrointestinal (GI) cancers.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Since 2013, Cleveland Clinic’s Digestive Disease & Surgery Institute has offered endoscopic submucosal dissection (ESD) as an alternative to traditional surgical treatment of early-stage gastric and esophageal tumors.
This minimally invasive technique was introduced to Cleveland Clinic for use with esophageal and gastric cancers by gastroenterologist Amit Bhatt, MD. Dr. Bhatt received grants from the American Society for Gastrointestinal Endoscopy and the American College of Gastroenterology to complete extensive ESD training in Japan, where the technique was originally developed and perfected.
“ESD was initially developed to address the high incidence of gastric cancers in Japan, but due to its success, it was later extended to treat esophageal and colonic tumors as well,” says Dr. Bhatt. “The goal of the procedure is to provide a high curative resection rate, while preserving the patient’s quality of life.”
At the 2019 Digestive Disease Week (DDW) annual meeting in San Diego, he lectured and conducted a hands-on ESD workshop for physicians interested in learning more about the procedure.
Dr. Bhatt and his colleagues also presented preliminary results from a large multi-center study comparing outcomes of ESD versus endoscopic mucosal resection (EMR) for treating Barrett’s esophagus-associated neoplasia. They found that ESD provides more definitive therapy than EMR. EMR is associated with significantly higher 12-month local recurrence rates than ESD (63% and 11%, respectively; p < .0001). Final results will be presented at the American College of Gastroenterology’s 2019 annual scientific meeting in October.
ESD employs specialized tools via a standard upper endoscope through the mouth to remove benign or malignant lesions of the esophagus and stomach. Most patients are discharged shortly after the procedure, or following an overnight stay.
Thus far, Dr. Bhatt and his colleagues have had excellent results with ESD in patients treated at Cleveland Clinic.
“In the past five years, we’ve had a greater than 90% curative resection rate for patients who underwent ESD for esophageal and gastric cancer,” says Dr. Bhatt. “We’ve had no perforations or major complications as consequences of this procedure. ESD has really changed the lives of many patients we have treated, including those who were not candidates for conventional surgery and who would not otherwise have been able to receive curative treatment.”
Dr. Bhatt notes that the one disadvantage of ESD compared to traditional surgery is that it cannot be used to remove lymph nodes on the exterior surfaces of the esophagus or stomach.
“For this reason, endoscopic resection should only be performed on isolated tumors that have not spread beyond the gastrointestinal tract,” he says. “Selecting the right patient for ESD is critical to the procedure’s success, which is why we use a multidisciplinary approach to evaluate each patient.”
At Cleveland Clinic, all ESD candidates undergo a comprehensive evaluation by Dr. Bhatt, an oncologist and a surgeon, during which the team reviews all options with the patient to develop a treatment plan.
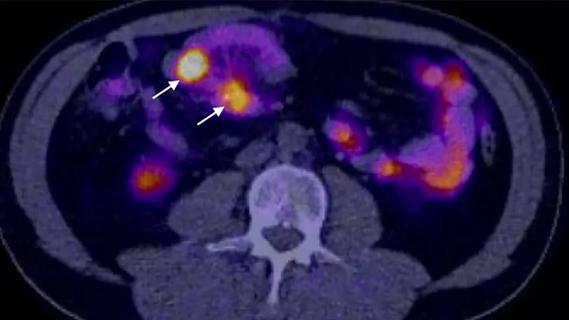
The evaluation also includes complete cancer staging using endoscopic ultrasound and computed tomography/positron emission tomography scans. Following the ESD procedure, patients continue to undergo periodic surveillance.
“We really take ownership of our patients and try our best to become their medical home where they will continue to come back for follow-up,” says Dr. Bhatt. “This is a major part of our success with ESD. By having patients return for surveillance, we are able to keep a close eye on those who may be at risk for recurrence or who need additional care. ESD is a technically challenging procedure and it is very important that the procedure be performed by a care team that has the training, expertise and patient volume needed for a good outcome.”
Dr. Bhatt said his DDW lecture and hands-on demonstration of ESD were motivated by the need to encourage and train additional ESD specialists in the U.S.
“We want to equip other physicians with the tools and knowledge to do this procedure and benefit patients on a wider scale,” he says. “In the talk, I shared our experiences with ESD, the training required for this procedure and criteria for patient selection. In the hands-on course, we trained interested physicians from around the world on how to do ESD using an ex vivo porcine model.”
To date, Dr. Bhatt and his colleagues have performed hundreds of ESD procedures at Cleveland Clinic. Endoscopy fellows there receive ESD training as part of their fellowship training.
Image: Endoscopic submucosal dissection — cutting around the outside of the tumor margin. © Cleveland Clinic Foundation.

An underdiagnosed condition in patients with cancer
Study demonstrates superior visualization of occult primary lesions

New device offers greater tumor control for malignant liver lesions
Cleveland Clinic researchers discover what drives – and what may halt – virus-induced cancer

First-ever U.S. population-level retrospective analysis reveals many patients with systemic mastocytosis need faster intervention

New program provides prehabilitation and rehabilitation services to help patients with cancer maintain and regain function

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients