Study finds postoperative pain is associated with early breastfeeding, length of stay and postpartum depression

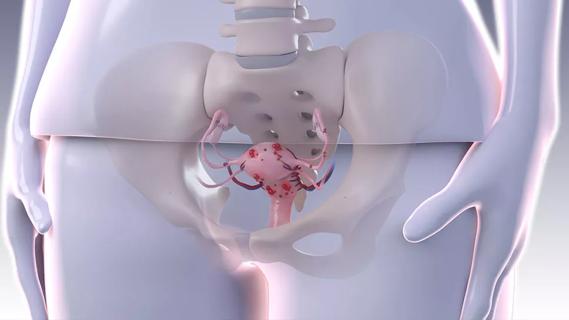
Adequate pain control following cesarean delivery is associated with a variety of outcomes, including breastfeeding initiation, length of stay and postpartum depression, according to a recent study published in the Journal of Clinical Anesthesia.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In clinical practice, we do see an association between increased postoperative pain and decreased breastfeeding success,” says Jennifer Eaton, DO, of Cleveland Clinic’s Ob/Gyn & Women’s Health Institute, who was not involved in the study. “By keeping pain under control during and after cesarean delivery, mothers and babies are much more likely to enjoy early bonding time, which is important for outcomes like breastfeeding and neurodevelopment.”
“In this study, we sought to determine the association between postoperative pain and breastfeeding during the hospital stay,” says senior author Alparslan Turan, MD, Vice Chairman of Outcomes Research and Staff at Cleveland Clinic’s Anesthesiology Institute. “We looked at this early postpartum period because studies indicate that early breastfeeding (i.e., within the first hour of delivery) is associated with successful exclusive breastfeeding, which has health and wellbeing benefits for both mother and baby. We were curious to see if poorly controlled postoperative pain impacted exclusive in-hospital breastfeeding rates.”
Researchers analyzed data from 5,350 adult patients who underwent a scheduled cesarean delivery following a singleton intrauterine pregnancy under spinal anesthesia. The procedures were conducted at a single institution between 2013 and 2016. Patients unable to breastfeed for maternal reasons (e.g., communicable illness, intensive care admission) or infant reasons (e.g., anatomic issues or admission to neonatal intensive care unit) were excluded from this analysis, as were chronic pain patients taking pain medications.
To document postoperative pain levels, nurses recorded a patient’s pain levels using a standard, 11-point numeric rating scale (NRS-11) every 15 minutes in the postanesthesia recovery unit and then every 2-4 hours throughout the remainder of the hospital stay. Early breastfeeding effectiveness was determined using the LATCH (Latch, Audible swallowing, Type of nipple, Comfort, and Hold/help) score. We found that higher pain scores were associated with lower LATCH scores (p < 0.04). Additionally, every one point increase in the average pain score significantly reduced the odds of mixed-feeding or exclusive breast feeding relative to exclusive formula feeding.
“We found that postpartum pain had a quite significant impact on in-hospital breastfeeding,” says Dr. Turan. Other variables were also associated with reduced in-hospital breastfeeding including maternal age and BMI, and APGAR5 scores.
“We also used the available data to determine if there were associations between post cesarean pain and length of stay or postpartum depression,” says Dr. Turan.
Analysis of these variables found associations between average pain score and both length of stay and postpartum depression. In terms of length of stay, for every one point increase in average postpartum pain on the NRS-11 pain scale, there was a corresponding increase of nearly one day in the length of stay (p < 0.0001). Mothers diagnosed with postpartum depression within one month of discharge had higher maximum pain scores (i.e., 7.66 [95% CI: 7.45–7.88]) than those who were not diagnosed with post-partum depression (i.e., 7.22 [95% CI: 7.18–7.26]).
“It is difficult to determine the clinical significance of the association between postoperative pain and postpartum depression,” Dr. Turan cautions. “We don’t usually know the exact reason a woman develops postpartum depression, but we do see a significant association with pain. Uncontrolled pain is a big stressor, which may contribute to depression. However, it is difficult to determine causality here. Perhaps a woman is having pain and the pain contributes to her depression, or perhaps a woman is depressed and that contributes to her experience of pain. Nonetheless, the association is clear.”
“The biggest takeaway from our study is that adequate pain control after cesarean delivery is very important to the health and wellbeing of mom and baby, impacting successful breastfeeding as well as maternal mental health. Uncontrolled pain in the perioperative period can linger for a long time, and can become a chronic pain condition.”
At Cleveland Clinic, Ob/Gyns have worked together with anesthesiologists to overhaul the time-honored strategy of administering opioids following cesarean delivery. Poor pain control can make it difficult for new mothers to learn how to care for a newborn, prolong recovery and increase the likelihood of postpartum depression. However, opioid medication comes with severe side effects, including sluggishness, dizziness, nausea, vomiting, breathing issues and the potential for addiction.
“Our Anesthesia colleagues typically use neuroaxial blockades for cesarean sections, and add a long-acting intrathecal narcotic at the time of spinal/epidural placement, which extends pain relief for 18–24 hours,” Dr. Eaton explains. “The Anesthesia team treats the patients with 1000 mg of acetaminophen prior to surgery, and then administer 30 mg of IV ketorolac at the end of surgery.”
Patients transition to ibuprofen and acetaminophen every six hours on a staggered schedule throughout their post-operative recovery, according to Dr. Eaton. “We do prescribe oral narcotics on an as-needed basis; however, since we instituted this postoperative pain management protocol, the narcotic usage for post-operative pain is significantly decreased. In addition, fewer patients require prescriptions for narcotics at the time of discharge to home.”
“Perhaps the most important postoperative intervention we’ve instituted relates to patient education. In our birthing hospitals, a team of advanced practice providers round on postpartum patients daily. These providers help patients understand the pain management plan, and are able to gauge how well the regimen is working before discharge to ensure success at home.”

Comparing strategies for cesarean prophylaxis with penicillin allergy
Counseling and careful surgical considerations are key

Deprivation is linked to impaired glucose intolerance and racial disparities

Perioperative prophylaxis and class III obesity

Artesunate ointment is safe well and tolerated patients with vulvar intraepithelial neoplasia

Endoscopic balloon dilation during pregnancy helps optimize outcomes

Researchers examine waste and implore colleagues to take action

Mode of delivery does not affect patient satisfaction