Vasculitis is a growing complication of PID

Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
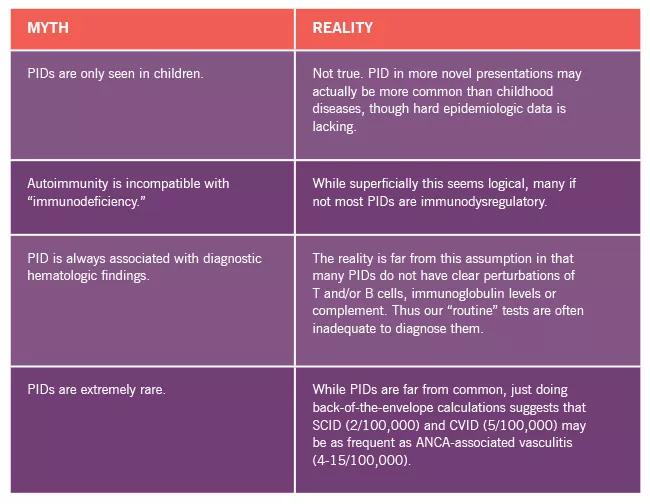
The rheumatologist who trained just a few years ago may still be laboring under the impression that primary immunodeficiency disorders (PID) are all about infection. In fact, there has been a renaissance in our thinking about PID that has busted a number of myths in addition to the belief that PIDs only manifest as infections. These include:
A more contemporary view of PID is displayed in the figure below, emphasizing the growing spectrum of noninfectious complications.
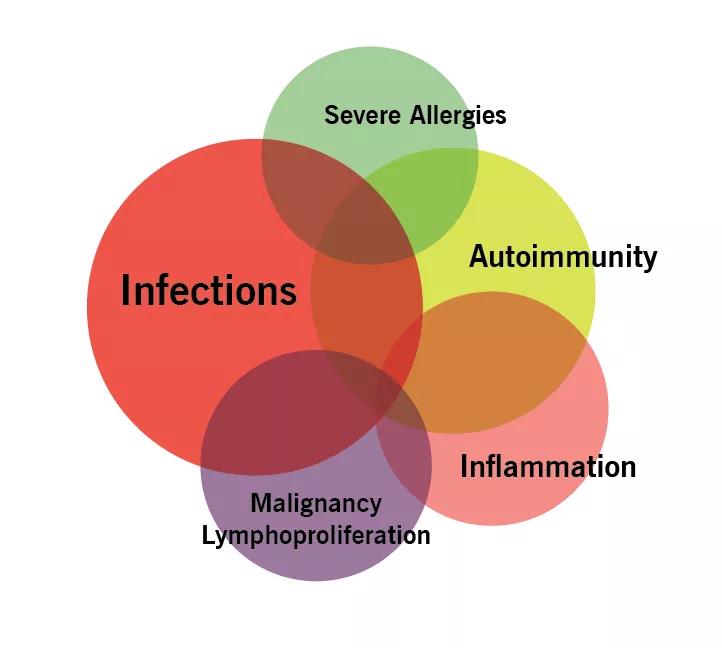
Among the autoimmune/inflammatory complications of PID are increasing cases of various forms of vasculitis. Until recently, these cases have been the subject of isolated case reports.
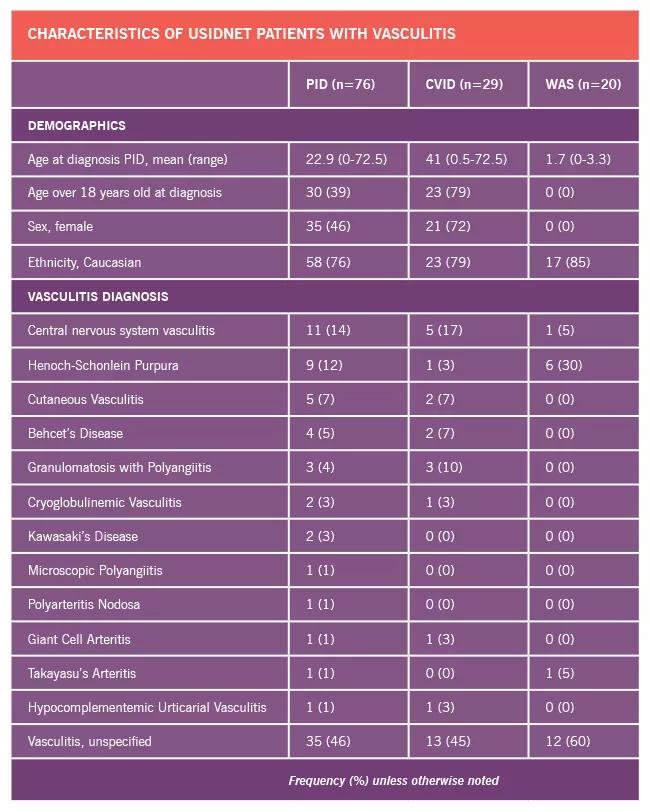
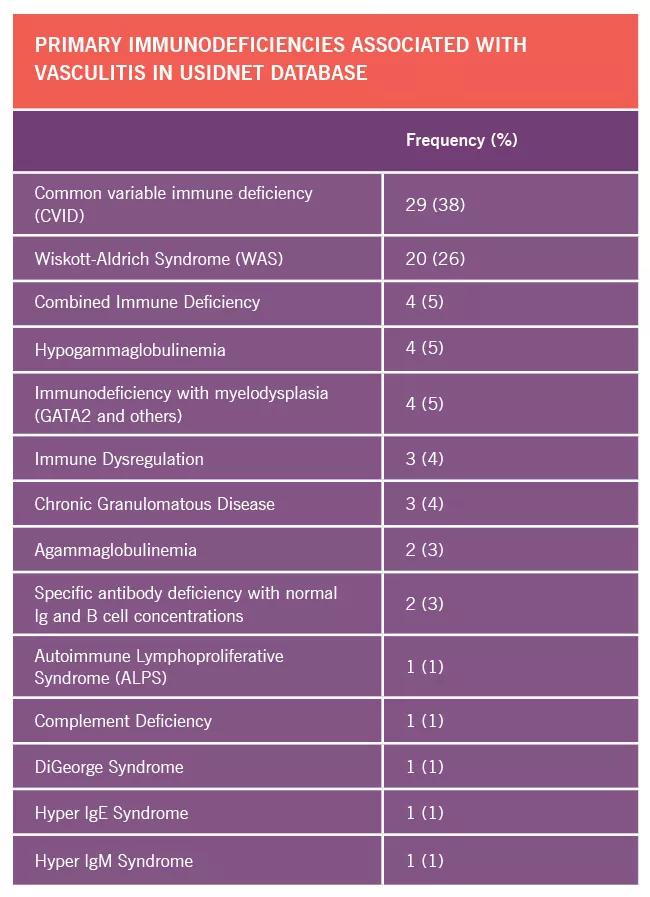
This year, Kevin Byram, MD, a vasculitis fellow working with James Fernandez, MD, PhD, who directs the adult immunodeficiency program in Cleveland Clinic’s R.J. Fasenmyer Center for Clinical Immunology, and I performed systematic query of the United States Immunodeficiency Network (USIDNET) database in an effort to get a clearer picture of the scope of the relationship between PID and vasculitis. USIDNET is a large, national consortium organized to collect registry data on patients with PID. The database has information on nearly 5,000 patients, and data regarding demographics, type of vasculitis diagnosis, specific PID diagnosis, immunologic laboratory results and immunomodulatory treatment was abstracted from the records.
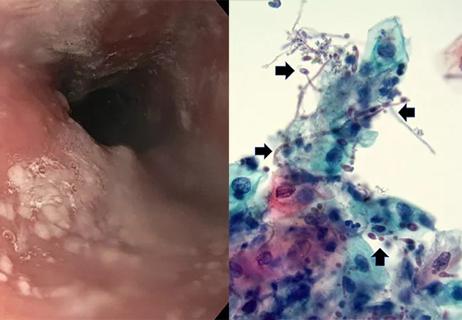
In total, 76 cases of vasculitis were identified, with the majority occurring in two disorders: common variable immunodeficiency (CVID) state, the most common adult form of PID, and Wiskott-Aldrich syndrome (WAS), a severe form of PID observed in children. Interestingly, a number of clinical forms of vasculitis were observed, but selective expression in the CNS was quite common. This is important since CNS vasculitis is a great mimicker of numerous conditions, including both neoplastic disorders and infections. Thus, in individuals with PID who may present with history of both, the diagnosis can be particularly challenging.
Dr. Byram presented on this topic at the 2018 ACR Annual Meeting in Chicago.
We are now working to address the etiopathogenesis of these associated disorders using the CNS vasculitis biobank run at Cleveland Clinic’s R.J. Fasenmyer Center for Clinical Immunology by Rula Hajj-Ali, MD, a noted authority in the CNS vasculitis space. In this project, samples of blood and cerebrospinal fluid are combined with informatics data of clinical findings and neuroimaging. Recently, the clinical use of next-generation sequencing has been added in the center’s diagnostic algorithm, and the results published in JAMA Neurology.
For rheumatologists, the takeaway is clear. First, look seriously at all patients with suspected CNS vasculitis for a history of PID. Of note is that in addition to the diagnosis discovered in the study above, many other PIDs can have CNS vascular involvement, including Aicardi-Goutieres syndrome, RAG deficiency and SATAT-1 hypermutation. Secondly, in patients with documented PID, isolated organ dysfunction (e.g., kidney, lung, heart, CNS) may be the consequence of vasculitis.
This is just the beginning of the exploration of a new and exciting field.
Dr. Calabrese is Director of the R.J. Fasenmyer Center for Clinical Immunology at Cleveland Clinic.
Advancements lead to a new trial involving autoimmune disease

Treatment strategies require understanding of pathomechanisms

Education, prevention strategies and monitoring serves this at-risk group
Treatment for scleroderma can sometimes cause esophageal symptoms

Lupus Clinic providers collaborate to advance treatment and understanding

Symptoms complement one another

Collaboration was key to identifying source of nerve condition

A review of expanding options that hold new promise