Coordinated interdisciplinary approach is key to success

A new study published in Headache finds a distinctive Cleveland Clinic outpatient rehabilitation program improved pain and functioning as well as reduced psychological impairment in patients previously debilitated by chronic headaches. Significant gains were evident both at discharge and a year later.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Known as IMATCH (Interdisciplinary Method for the Assessment and Treatment of Chronic Headache), the program involves intensive treatment incorporating medication management, patient education about headache, relaxation training, counseling and exercise. Participants undergo eight hours of daily outpatient treatment five days a week over a three-week period.
“Our program has proven successful in helping patients who often have lived for years with extreme disability from chronic headaches that had been refractory to outpatient management,” says Steven J. Krause, PhD, MBA, lead author of the study and director of the IMATCH Program. “Most are able to regain function and achieve other important benefits — and retain their gains long-term.”
The IMATCH program, run out of Cleveland Clinic’s Center for Neurological Restoration, started in January 2007 and has treated about 1,000 patients. Dr. Krause, a clinical psychologist specializing in pain management, notes that IMATCH is distinctive because virtually all other U.S. programs that achieve comparable results for chronic headache are inpatient programs, which are much costlier to run and often less convenient for patients.
Dr. Krause’s study was a prospective cohort investigation involving 379 consecutive chronic headache patients admitted to the IMATCH program. Inclusion criteria required that patients regularly suffered significant functional impairment or emotional distress from headaches or maintained functioning only with the inappropriate use of medications. The most common diagnoses on admission were migraine and substance- or withdrawal-related headache.
The study assessed program participants with a variety of self-report questionnaires at the time of admission (N = 371), at discharge (N = 340) and at one-year follow-up (N = 152).
Function was measured by the Headache Impact Test (HIT-6) and the Pain Disability Index, both indicators of the impact headaches have on ability to function at work/school/home and socially. Results showed substantial improvement, from mean scores indicating moderate disability at program entry to mild disability at discharge, with continued improvement a year later.
Pain was ranked by patients on a 10-point scale. Average pain improved from a mean of 6.1 at admission to 3.5 at discharge and 3.3 at one-year follow-up. Similar trends were observed for estimates of worst pain in the prior month, least pain in the prior month and current pain.
Psychological status was measured by the Depression Anxiety Stress Scales (DASS-42), a 42-item self-report inventory. In all categories, measures significantly improved from the beginning to the end of the program, with mean scores at discharge and at one year in the normal range for each category.
Dr. Krause emphasizes that helping patients improve function, rather than curing pain, is the primary goal of the IMATCH program. The disability that many patients with chronic headache experience is severe, he notes, saying that “some are stuck in bed 24/7.”
Unlike acute pain, chronic pain is particularly difficult to control, and IMATCH patients have usually undergone multiple prior attempts to stop their pain, Dr. Krause explains. Although patients are told that IMATCH will focus on regaining function rather than curing pain, the study showed that the program did prove effective in reducing pain — as well as in improving psychological factors that frequently afflict patients with chronic pain.
Dr. Krause credits the program’s success to its integrated approach to chronic headache management, combining multiple avenues of therapy, including medicine, nursing, psychology and physical therapy.
“Patients arrive with multiple, overlapping problems, not just headache,” he says. “Depression, anxiety, excessive prescriptions and social withdrawal all play important roles in their reduced functioning. While one could set up a patient with individual services to address these problems, the interdisciplinary coordination makes a huge difference in our ability to make rapid progress.”
He likens treating chronic headache to subduing an octopus. “If you pin down only one arm, the others will reach out to get you,” he says, adding that most patients entering the program have already seen multiple specialists who have treated “only one arm of the octopus” at a time.
How long improvement can be maintained is an interesting avenue of future research, says Dr. Krause. He adds that gathering long-term follow-up data is an important challenge.
He also suspects that patients with certain diagnoses are more amenable to specific types of interventions, and that future efforts should try to tease out such factors with the goal of “more effectively choosing treatments for each unique patient.”

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

New grant-funded investigation illustrates impact and reach of Cleveland Clinic Brain Study
How the new longitudinal investigation could become the Framingham Heart Study of brain health

Pilot findings show good patient acceptance and safety, early hints of efficacy

Study finds high prevalence of symptoms, willingness to seek treatment
Panel outlines research priorities around a promising alternative to imaging markers
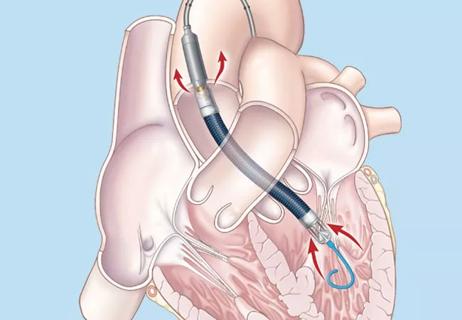
Suspected factors include antithrombotic intensity, time on device, presence of thrombocytopenia

Preclinical studies will assess whether method developed for stroke recovery curbs deficits after brain injury