Association highlights importance of the nose in infection
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The nose seems to be the major port of entry for severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Nasal swabs detect higher viral loads compared with throat swabs, and the highest expression of Angiotensin Converting Enzyme 2 (ACE2), which the virus’ spike protein engages as the entry receptor, is in the nose. Given the nose’s critical role in the pandemic, our group recently conducted a study in association with Ronald Strauss, MD, from the Cleveland Allergy and Asthma Center to determine whether intranasal corticosteroid (INCS) use suppresses viral load and receptor expression and is thus protective against hospitalization and death from Coronavirus Disease 2019 (COVID-19).
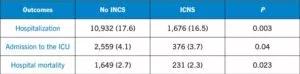
In a study funded by the National Heart, Lung and Blood Institute and the National Institute of Neurological Disorders and Stroke, our research team used the Cleveland Clinic COVID-19 Research Registry (CCCRR) to perform a propensity score matching for INCS treatment prior to infection with SARS-CoV-2 in 72,147 patients. These patients were registered from April 1, 2020 through March 31, 2021 at Cleveland Clinic. We measured endpoints of hospitalization, intensive care unit (ICU) admission and in-hospital mortality.
Just over 17% of patients were hospitalized, and about a third of those (4.1% of total) required ICU admission. A little over half of the patients admitted to the ICU died during hospitalization, 2.6% of included patients. Fourteen percent of the overall cohort was utilizing INCS prior to SARS-CoV-2 infection (N = 10,187). Patients who used INCS were a bit older (52.07 vs. 50.33 years) and more likely to be female (64% vs. 53.3%) than nonusers.
When compared with peers, users of INCS reported more symptoms but had lower risk for hospitalization (adjusted OR [95% CI]: 0.78 [0.72-0.85]), admission to the ICU (adjusted OR [95% CI]: 0.77 [0.65-0.92]) and in-hospital death (adjusted OR [95% CI]: 0.76 [0.61-0.94]). In a sensitivity analysis, we were able to replicate findings after excluding patients on inhaled corticosteroids (iCS) and with allergic rhinitis. The positive impact of INCS remained significant after adjusting for pre-infection baseline blood eosinophil count in a subset of 30,289 patients.
Previous studies have shown that patients with allergic rhinitis or asthma were hospitalized and ventilated less often, but those studies did not control for the use of iCS and absolute eosinophil counts. Adjusting for iCS usage is a crucial step, as it has been linked to decreased ACE2 expression in vitro. Our study is particularly significant because it demonstrates continued benefits after these adjustments.
The dominance of the B.1.617.2 variant, which has an even higher concentration of viral load in the nasal passages, brings a particular sense of urgency to corroborate our data through a randomized clinical trial. If INCS use is indeed protective, we could reduce hospitalizations, mortality and healthcare resource utilization with an over-the-counter, well tolerated and low cost tool. However, until we have the necessary data and approval, INCS cannot be recommended to prevent or treat COVID-19 at this time.
Dr. Zein is staff in the Department of Pulmonary Medicine.
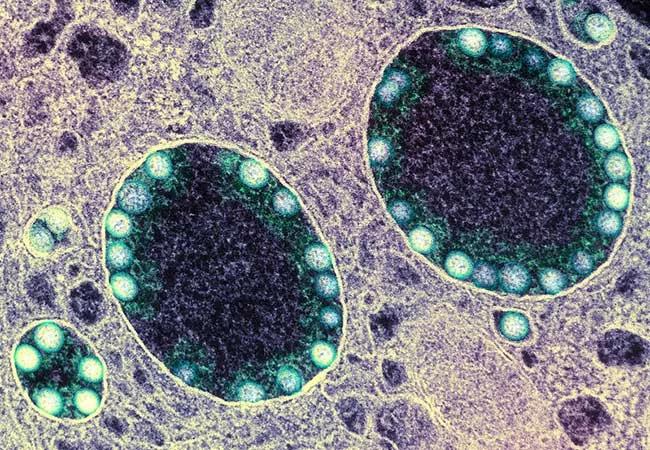
Image: Transmission electron micrograph of SARS-CoV-2 virus particles (teal) within endosomes of a heavily infected nasal olfactory epithelial cell. Image captured at the NIAID Integrated Research Facility in Fort Detrick, MD. Credit: NIAID.

Patients report improved sense of smell and taste

Clinicians who are accustomed to uncertainty can do well by patients

Unique skin changes can occur after infection or vaccine

Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition
As the pandemic evolves, rheumatologists must continue to be mindful of most vulnerable patients

Early results suggest positive outcomes from COVID-19 PrEP treatment

Could the virus have caused the condition or triggered previously undiagnosed disease?

Five categories of cutaneous abnormalities are associated with COVID-19