Collaborative efforts that are shaping best practices

Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As a specialist in pediatric infectious diseases, I care for and treat children with various types of infections. For children admitted to the hospital for surgery, treatment of cancer or management of another illness, the hospital should be a safe environment where healing occurs free from complications.
Healthcare-associated infections are a particularly unfortunate complication of treatment because they result in significant morbidity, sometimes mortality, and are largely preventable with adherence to best practices. Common healthcare-associated infections that occur in hospitalized children include surgical site infections (SSIs), catheter-associated urinary tract infections (CAUTI) and central line-associated bloodstream infections (CLABSIs).
I work closely with a diverse group of care providers, both within our own children’s hospital and at peer institutions, in my role as Medical Director for Pediatric Infection Prevention at Cleveland Clinic Children’s. These providers work diligently to implement and share best practice measures and cultural improvements to help prevent hospital-acquired infections.
My own involvement in this journey began in 2009 through our hospital’s participation in the Ohio Children’s Hospitals’ Solution for Patient Safety (SPS) network, a network of eight children’s hospitals that came together to promote the implementation of high-reliability organization principles, data transparency and the sharing of best practices that improve safety processes and culture.1
Measures promoted at our institution included appropriate prophylactic antibiotic choice, on time delivery of the antibiotic and chlorhexidine bathing. To facilitate our efforts, we created an automated database that allowed us to track in a procedure-specific manner compliant with the best practice process measures promoted by the collaborative.
In children undergoing spine fusion procedures, we found that antibiotic choice, an easily modifiable variable, was associated with SSI risk at both 90 days and during prolonged surveillance, a definition that also includes later occurring infections (Figure 1).
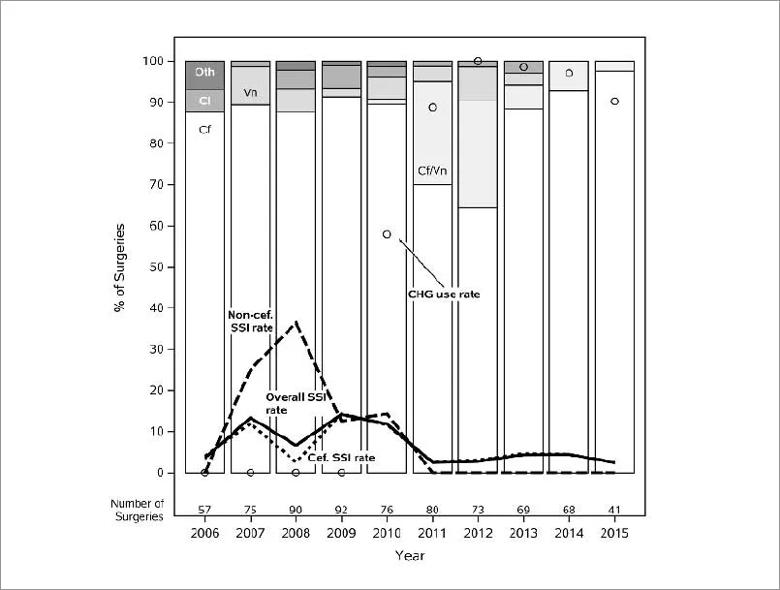
Figure 1. Annual Rate of Prophylaxis with Various Antibiotic Regimens and Preoperative Chlorhexidine Use in Pediatric Spine Fusion and the Rate of Surgical Site Infection (SSI). Antibiotic and chlorhexidine (CHG) use rates are expressed according to the regimen used, as the percent of the total number of surgeries. Antibiotic regimens (N=721) included cefazolin monotherapy (Cf), cefazolin plus vancomycin (Cf/Vn), vancomycin monotherapy (Vn), clindamycin monotherapy (Cl) or other (Oth). SSI rates (Overall SSI rate) are based on a prolonged surveillance definition that includes all infections that required wound washout or exploration, regardless of time from surgery. SSI rates are stratified according to whether the regimen included cefazolin (Cef. SSI rate). Acknowledgement: Ritika Coelho, MD and Sarah Worley, MS.
Cefazolin-containing regimens were associated with lower 90 day (12.5% vs 3.9%; P = 0.01) and prolonged surveillance (14.3% vs 6.4%; P = 0.05) SSI rates than non-cefazolin containing regimens, most often vancomycin or clindamycin monotherapy.
We promoted the safe use of optimal cefazolin-containing regimens and observed a decline in both early and late SSIs. We still use the database in an optimized format to ensure continued compliance with prophylactic antibiotic guidelines, to explore risk factors for SSIs in unique populations, such as neonates, and to develop tools for automating SSI surveillance.
The ongoing challenge, however, is that no single children’s hospital cares for enough patients to obtain sufficient data to allow for a reliable assessment of whether process measures aimed at preventing harm are actually achieving that goal.
However, the expansion of the SPS network from eight Ohio children’s hospitals to more than 145 children’s hospitals provides an opportunity to look broadly at the incidence of CAUTI and implement prevention measures across the network.2,3
Although CAUTI insertion and maintenance bundles had been used in adult populations and studied in individual children’s hospitals, there was a need to demonstrate their efficacy in a large pediatric population.
Together with collaborators at SPS, we reviewed the literature and surveyed participating hospitals to determine best practice methods for preventing CAUTI. Ultimately, we decided that the insertion and maintenance bundles used for adults were suitable for implementation in pediatric populations.
After the introduction of the SPS CAUTI prevention bundles, the CAUTI rate across the network decreased 61.6%, from 2.55 to 0.98 infections per 1,000 central line days (Figure 2).
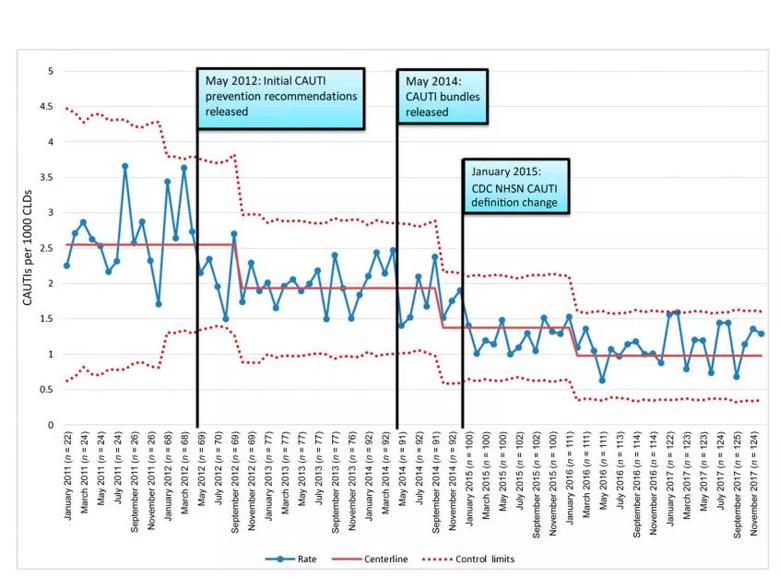
Figure 2. SPS network aggregate CAUTI rate. The number of CAUTIs per 1000 CLDs is plotted monthly on a u-chart, in which n is the number of hospitals reporting data for that month (every other month is reported for ease of display). Dates for key events include May 2012, release of SPS recommended bundle; May 2014, release of SPS bundle and evidence; and January 2015, CDC NHSN CAUTI definition change. The yellow line denotes the centerline. The blue line with dots denotes CAUTI rate. The red dashed line denotes control limits. Readjustment of the centerline required 8 consecutive points above or below the centerline. Reproduced with permission Pediatrics.3
CLABSIs are arguably the most important healthcare-associated infection, and justifiably hospitals have devoted significant resources to implement harm prevention measures. The key to the prevention of CLABSIs is care bundles aimed at minimizing the risk of introducing an infection at the time of line insertion or maintenance.
Some children only have central lines in place during their inpatient hospital stay, while others, like those receiving treatment for cancers, have the central line in place for months. It facilitates the delivery of lifesaving chemotherapies, nutritional and blood support, and enables the transition of care to an outpatient setting.
To better understand the overall risk associated with central line use, we explored CLABSIs and non-CLABSI central venous catheter harm events (CLANCs) over 10 years in 366 children and young adults who received cancer treatment. Our findings showed that inpatient CLABSIs accounted for only 22% of the harm events (Table 1).
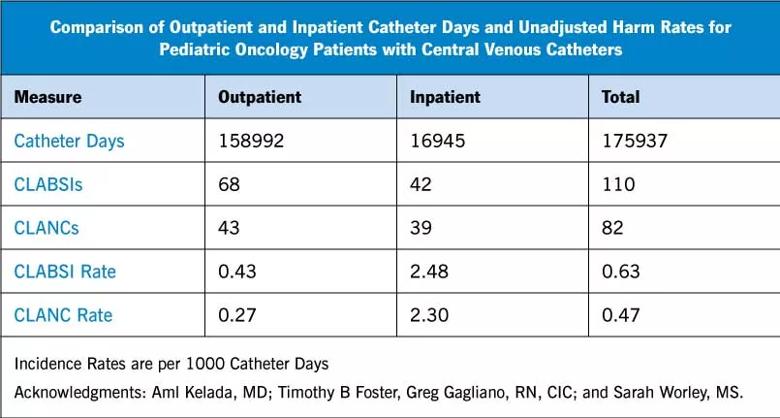
Half of all CLABSIs occurred among outpatients, and CLANC complications occurred at rates similar to CLABSIs. Two groups of patients were at especially high risk of developing both CLABSIs and CLANCs—those with acute myeloid leukemia and infants.
Lines with more than one lumen were at especially high risk for developing CLABSIs and lines placed during infancy were associated with a higher CLANC risk, especially catheter dislodgement. These findings highlight not only the importance of outpatient CLABSIs but also the importance of noninfectious catheter complications. The role of the line choice is of key importance in the prevention of downstream harm and the need to develop improved techniques, especially in infants, to prevent noninfectious complications such as catheter dislodgement.
These findings will perhaps lead to best practices that can be shared with other children’s hospitals.
From my practice of pediatric infectious diseases, I am able to recall many patients with infections that I have helped treat. As I reflect on my contributions, the greatest satisfaction comes, however, from working with my local colleagues and peers at other hospitals on collaborative projects aimed at preventing healthcare-associated harm.
In infection prevention, we do not typically meet the children who never develop postoperative wound infections, CAUTIs or CLABSIs. It is well that we did not meet.
References
About the author: Dr. Foster is Medical Director of Pediatric Infection Prevention at Cleveland Clinic Children’s and Associate Professor of Pediatrics, Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
Why timely screening and treatment are needed

Managing care and counseling your patients

Primarily a pediatric phenomenon, co-infection alters the disease course

Unpacking advancements and identifying drivers of inequity

Self-efficacy mindset, burst therapy and increased biofeedback may help improve outcomes

Pediatric and adult gastroenterologists offer team care for patients with eosinophilic esophagitis

New guidelines expand on psychosocial, sexual health, cognitive and other issues

Consensus conference begins work on new recommendations for clinical care and research