Children may present with hyperinflammatory responses similar to Kawasaki disease or toxic shock

Reports of pediatric patients developing symptoms of Kawasaki disease after COVID-19 are a reminder that children do face risks from the virus. But while these cases have received public attention, severe outcomes from COVID-19 in children are still rare, says Frank Esper, MD, a pediatric infectious disease specialist at Cleveland Clinic Children’s.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Pediatrics has, for the most part, been spared,” he says. “But that doesn’t mean there are no problems. Children can get sick. Children have died of COVID-19. And children have shown up with this very unusual manifestation of hyperinflammation.”
There’s still much that’s unknown about how COVID-19 affects children, he adds, but that will likely start to change as hospitals reopen to more patients, resulting in increased testing and a more accurate count of pediatric cases.
New York City released a bulletin on May 4 after 15 children with COVID-19 were hospitalized with persistent fever and hyperinflammatory response similar to Kawasaki disease. That followed a warning issued by British health officials in April after similar cases were reported there.
But with just a few dozen such reports out of what’s likely hundreds of thousands of COVID-19 cases, “it’s probably very rare,” Dr. Esper says. “I would still say that the vast majority of children have mild symptoms with COVID-19. However, I would also say that we’re still in the process of recognizing what the symptoms in children are.”
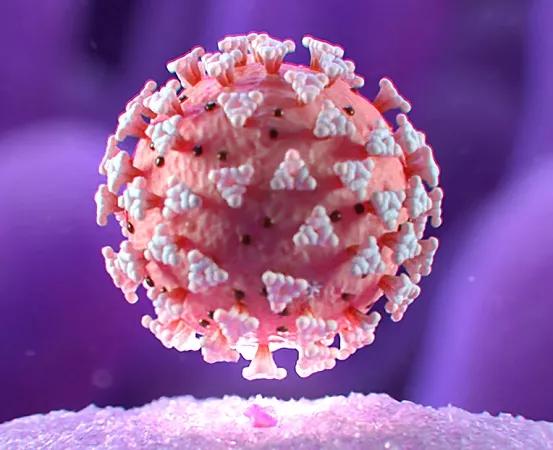
One type of hyperinflammatory response, the cytokine storm, has been a known complication in adult patients with COVID-19, and these cases could be a childhood variant, he adds.
Pediatricians are well aware of the symptoms of Kawasaki disease, including high fever, flushed skin and eyes, rash, swollen hands and feet, “strawberry tongue,” and bloodwork indicating an extremely high inflammatory response. “It’s a specter in pediatrics,” says Dr. Esper. “Nobody knows what causes it or why people get as sick as they do, but we do know how to treat it.”
Other conditions can cause a similar hyperinflammatory response, including other infections, toxic shock syndrome and severe allergic reactions to medications. With these new reports, physicians should be aware that COVID-19 is another possible cause, says Dr. Esper. “I’m going to add it to the list of things that can lead to this clinical presentation of hyperinflammation,” he says.
Clinical guidance on how to treat these symptoms hasn’t changed — but it might, as scientists learn more about how the virus works in adults and children and find medications that help fight the disease and its complications, he says.
It’s already known that some symptoms like hyperinflammation, diarrhea and gastrointestinal issues, and “COVID toes” are more prominent in children than in adults. With resources and attention focused on the sickest patients and those at highest risk, there has not been rigorous testing of children so far, he says. Consequently, there is little data around questions like how prevalent the virus is in pediatrics, and how it manifests in children.
That’s likely to change as hospitals that cleared beds to make room for a COVID-19 surge start reopening to more patients, and testing becomes more widely available, Dr. Esper says. Antibody testing could also reveal a large number of children who were infected but asymptomatic, he adds.
“As we start finding more and more children with COVID-19 — not because the virus is changing, but because we’re doing more testing — then I think we’re going to start learning a lot more about what this virus means for children,” he says. “I expect that we’ll learn that some of these things that flew under the radar we just didn’t recognize were being caused by COVID-19.”

Patients report improved sense of smell and taste

Clinicians who are accustomed to uncertainty can do well by patients

Unique skin changes can occur after infection or vaccine

Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition
As the pandemic evolves, rheumatologists must continue to be mindful of most vulnerable patients

Early results suggest positive outcomes from COVID-19 PrEP treatment

Could the virus have caused the condition or triggered previously undiagnosed disease?

Five categories of cutaneous abnormalities are associated with COVID-19