Secretome may yield therapy to maintain renal function

Prolonged interruption of renal blood supply from renal artery clamping during partial nephrectomy, followed by reperfusion, can cause tissue injury and necrosis, resulting in organ dysfunction and chronic kidney disease. Effective therapies for renal ischemia-reperfusion injury (IRI) are lacking and urgently needed.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Utilizing a rat model of IRI, new Cleveland Clinic research led by Margot Damaser, PhD, shows that mesenchymal stem cell (MSC) secretions improve recovery of renal function, and reveals some facets of how the secretions produce that beneficial effect.
“This work demonstrates that the secretions of stem cells may provide a real therapy to maintain renal function at the time of partial nephrectomy for kidney cancer,” Dr. Damaser says. “Thus, this therapy has the potential for enabling full renal recovery after clamping of the blood supply to the kidney, as is necessary to remove the cancerous portion.
The research was presented at the 2019 annual meeting of the American Urological Association (AUA).
MSCs are a type of mature stem cell found in bone marrow and almost all well-vascularized tissue. Their capacity for proliferation and differentiation into multiple terminal cell types, as well as the therapeutic potential of the acellular bioactive molecules they secrete, make MSCs a target of great interest in regenerative medicine, particularly in urologic applications.
MSCs’ regenerative properties, though not fully understood, show promise in treating diseases and conditions for which medical and surgical approaches are ineffective.
Initial attention focused on MSCs’ ability to differentiate and engraft to repair or replace damaged host tissue. Such incorporation and differentiation at the injury site appears rare, suggesting other therapeutic modalities may be involved.
More recently, Dr. Damaser and other researchers have been investigating MSCs’ varied and complex array of locally or systemically secreted soluble bioactive molecules. These trophic molecules, including growth factors, cytokines and hormones — collectively known as the secretome — have anti-inflammatory, antifibroitc, pro-angiogenic and anti-apoptotic properties that support regeneration, but without traditional stem cell therapy’s risk of oncogenic transformation and immunoreactivity.
Modification and therapeutic application of MSC secretome components could, in theory, serve as a customized regenerative drug delivery system to improve outcomes in various conditions. Preclinical studies by Dr. Damaser and others have shown the MSC secretome’s efficacy in several animal models of urologic disorders, including stress urinary incontinence, kidney disease and bladder/erectile dysfunction.
The two studies Dr. Damaser and colleagues presented at the AUA annual meeting described their efforts to further characterize the MSC secretome and use it to mitigate loss of kidney function following IRI. The pathophysiology of IRI is complex and incompletely understood. It can occur after infarction, sepsis, organ transplantation, or renal artery clamping during partial nephrectomy. No current therapies exist to prevent renal IRI, which induces acute kidney injury and contributes to high morbidity and mortality.
To investigate MSC secretions’ regenerative potential, the Cleveland Clinic researchers harvested bone marrow from Sprague-Dawley rats to obtain and grow MSCs in culture. Centrifuging and filtering produced a concentrated acellular solution of MSC-conditioned culture media (CCM).
In the initial study, the researchers created an animal model of IRI by clamping the left renal hilum for 45 minutes in Sprague-Dawley rats that had previously undergone right nephrectomy. Five minutes before clamping, the rats were intravenously administered either normal saline, non-conditioned plain media or CCM. To determine whether an alternate route of CCM administration affected outcomes, a second group of renal ischemia-reperfusion-injured rats received either intravenous normal saline, intravenous CCM, subcutaneous CCM or intra-arterial CCM. The rats’ serum creatinine (SCr), whose level over baseline is a marker for acute kidney injury, was measured on multiple days post-IRI. The rats’ kidneys were harvested 14 days post-IRI for histopathology.
Among the first rat cohort, by day 7 post-IRI, the animals that received CCM had significantly lower SCr relative to baseline than those that received saline or plain media (115% v 147%, p = 0.04; 115% v 151%, p = 0.02; respectively). In the second rat cohort, by day 14 post-IRI, the animals that received either intra-arterial CCM or subcutaneous CCM had significantly lower SCr relative to baseline than those that were untreated (114% v 224%, p = 0.03; 117% v 224%, p = 0.03; respectively). The kidneys of CCM-treated rats contained less tubular dilation and less loss of cellular structure than the kidneys of control animals.
In the follow-up study, Dr. Damaser and her colleagues sought to learn more about the mechanism of secretome-mediated renal IRI recovery. They focused on MSC-derived extracellular vesicles called exosomes, which are thought to contain some of the bioactive cytokines secreted by MSCs.
As before, the researchers used donor rat bone marrow MSC cultures to produce CCM. They isolated exosomes from the CCM using serial ultracentrifugation, and preserved the exosome-depleted CCM. Male rats underwent right nephrectomy and subsequent left renal hilum clamping to produce IRI. Five minutes before clamping, rats were administered either intravenous CCM, non-conditioned plain media, MSC-derived exosomes or exosome-depleted CCM. SCr levels were recorded on multiple days post-IRI.
All of the rats experienced a sharp SCr increase five days after IRI. By day 14, the rats treated with MSC-derived exosomes had significantly lower SCr relative to baseline than did the animals that received plain media (173% ± 20% vs 239% ± 11%, p = 0.008). Rats treated with exosome-depleted CCM or plain media had significantly higher SCr relative to baseline than animals that received CCM (130% ± 12% vs 191% ±17%, p = 0.007; 130% ± 12% vs 239% ±11%, p = 0.0002; respectively). Renal function at 14 days post-ISI as determined by SCr was not significantly different among the MSC-derived exosomes and exosome-depleted CCM groups (173% ±20% vs 190% ±17%, p > 0.05).
Taken together, the results of the two studies show that the acellular MSC secretome improves renal function after IRI. Since the improvement occurs regardless of the route the CCM is administered and both of the best performing routes are systemic rather than local, the effect is presumed to be via a systemic mechanism of action. And since MSC-derived exosomes specifically improve post-IRI renal function, that result shows that exosomes are partially responsible for mediating the therapeutic benefit.
“Both findings are noteworthy, and build on each other” Dr. Damaser says. “One demonstrates that we can provide treatment with the secretions of MSCs instead of the cells themselves, and we don’t have to administer treatment locally. Secrotome-based therapy may have cost benefits compared to traditional stem cell therapy, particularly since an off-the-shelf formulation may be given. Our other result begins to home in on the mechanism by which these secretions work, or at least what components are producing the therapeutic effect.”
Dr. Damaser’s current research focuses on tracking where the exosomes home or travel to, which would suggest how and where they are working to have their regenerative and reparative effects.
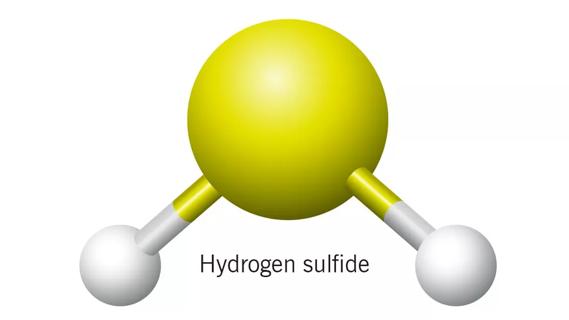
Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.
International collaboration is most genetically diverse study of the disease to date

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests
Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology

Research project aims to pinpoint biomarkers that could speed diagnosis