Holly L. Thacker, MD, weighs in
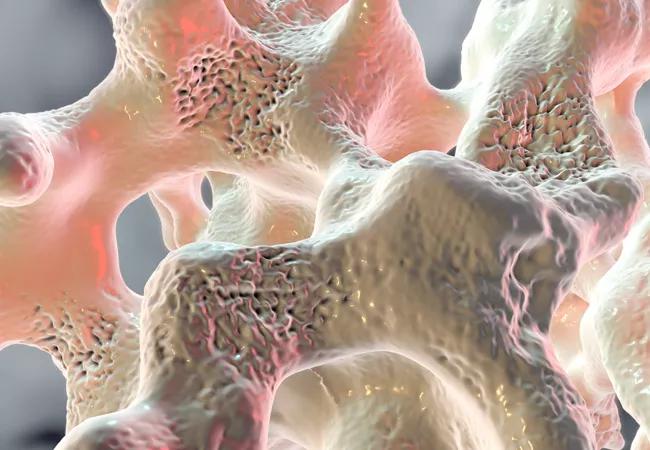
Up to 20 percent of bone loss occurs in women in their first five years of menopause. So it is imperative for physicians to discuss and institute a bone loss prevention plan when the first signs of menopause appear, says women’s health specialist Holly L. Thacker MD, FACP, Director, Cleveland Clinic Center for Specialized Women’s Health; Professor, Cleveland Clinic Lerner College of Medicine of Case Western Reserve University; and Executive Director of Speaking of Women’s Health.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Preventing fractures is critically important since hip fractures, for instance, significantly increase morbidity and mortality, and decrease quality of life in midlife women and beyond, and can lead to death or nursing home placement.
In this Q&A, Dr. Thacker helps physicians understand today’s osteoporosis prevention strategies.
Consult QD: When is it appropriate to use hormone therapy to prevent osteoporosis?
Dr. Thacker: Hormone replacement therapy (HT) is used to treat premature and early menopause — in women under age 40 to 45. For these women, HT is generally given at a higher dose than for postmenopausal women. HT for early menopause and after menopause helps the bone, and can help manage osteopenia and help prevent osteoporosis in women after menopause which is typically age 51.3 years. There is no time limit to the length of HT and HT only helps the bone while one is taking it.
The major risk of HT is venous thromboembolism, so if a woman is at risk for VTE, use only transdermal estrogen. If she is not at increased risk, use oral or transdermal.
And please prescribe estrogen for women with hysterectomy, especially those under age 65, which is good for bone and reduces diabetes, heart disease, death and breast cancer — and is underutilized. For symptomatic menopausal women with hot flashes and bone loss who have undergone a hysterectomy, use HT with estrogen.
To prevent osteoporosis in women with a uterus under age 65, I urge doctors to prescribe estrogen-progesterone therapy. Use “designer estrogen therapy,” which is estrogen and estrogen receptor agonist antagonist (ERAA) therapy or conjugated estrogens/bazedoxifene (DUAVEE®), for menopausal women with hot flashes and bone loss.
Five to 15 percent or more of women on HT can still lose bone density. This means that women on HT need to be monitored with periodic bone densitometry. Women with postmenopausal bone loss should have blood chemistries, including 25-OH vitamin D testing, thyroid-stimulating hormone/thyroid function and complete blood counts, and 24-hour urine collection for calcium assessment. Parathyroid hormone, serum protein electrophoresis, gluten celiac testing, 24-hour cortisol levels, and fasting urine NTX (N-terminal telopeptide) testing also can be useful.
The bottom line is that hormone therapy can be considered for bone health — in particular with concomitant menopausal symptoms that could be improved.
Women and providers do not need to be afraid of hormone therapy and there is no time limit for HT use. We just need the right dose and the right route for the right woman.
The North American Menopause Society’s 2017 Hormone Therapy Position Statement is a good resource that covers the benefits of HT for healthy postmenopausal women.
CQD: When do you recommend bisphosphonates?
Dr. Thacker: Physicians often prescribe bisphosphonates, such as alendronate (Fosamax®), zoledronic acid (Reclast®) or denosumab (Prolia®), for osteoporosis without considering that the woman has hot flashes, sleep disturbances, vaginal dryness and other conditions that would be helped with HT. So I recommend bisphosphonates for women with osteoporosis who have adequate renal function who do not want to take HT and/or in women on low dose HT who still lose bones.
Women on glucocorticoids should be considered for bone loss preventive therapy with bisphosphonates, because HT alone will not protect them against glucocorticoid-induced osteoporosis.
CQD: Are there other preventive or therapeutic options for osteoporosis?
Dr. Thacker: If a woman does not want or need hormone therapy, do not forget about daily ERAA, such as raloxifene, which is FDA approved to treat osteoporosis and reduces the risk of being diagnosed with ER-positive breast cancer.
For women with severe osteoporosis and/or fragility fractures, which constitutes clinical osteoporosis at the least, regardless of bone mineral density, then consider anabolic agents like teriparatide (Forteo®) or abaloparatide (Tymlos™). These are daily injectable medications used for 18-24 months, which are followed by IV either zoledronic acid or denosumab every six months.

Radiofrequency ablation significantly reduces symptom severity, shrinks nodules

Maternal-fetal medicine specialists, endocrinologists and educators team up

Giving young patients a hand as they take charge of their own health

Case illustrates how easily condition can mimic preeclampsia
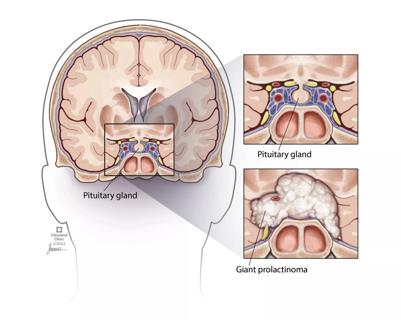
Analysis examines surgical resection of rare pituitary tumors
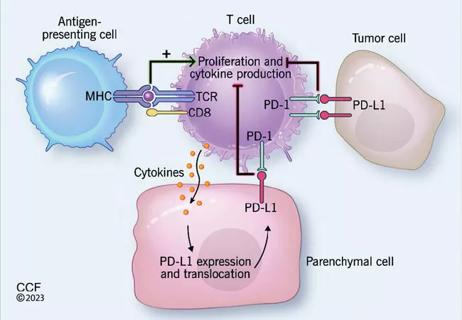
Screening and medication key to better outcomes

Spinal cord stimulation can help those who are optimized for success
Incidence, outcomes and management