Risk modification may be key

Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Atrial fibrillation (AF) affects more than 33 million individuals worldwide. In the United States and other industrial nations, the lifetime risk of developing AF is one in four from the age of 40. AF increases stroke risk fivefold, and there is also a twofold increased risk of dementia and increased risks of myocardial infarction (MI), heart failure and death.
Direct expenditures related to AF cost Medicare at least $6 billion annually, with indirect costs adding exponentially to the financial burden of this disease.
To date, most published AF studies have focused either on underlying mechanisms or clinical treatments of AF, with relatively few focused on AF prevention. The National Institutes of Health funded a 2008 meeting that began to address this important topic. With significant progress made since that time, the Heart Rhythm Society convened a December 2013 symposium focused on recent advances in the prevention of AF. A detailed summary of remaining knowledge gaps was published in Heart Rhythm in January 2015.
Prominent risk factors for the development of AF include hypertension, obesity, diabetes, heart failure and sleep apnea. To varying degrees, these contribute to most cases by forming a substrate for AF. The presence of nonmodifiable risk factors for AF—such as genetics, increasing age and height— can modulate the influence of modifiable risk factors.
While nothing can be done about the nonmodifiable risk factors, there is increasing evidence that efforts to control the modifiable risk factors can help to prevent the development of AF, or when AF is present, reduce the frequency and/or duration of AF episodes.
Frequent atrial ectopy (identified by Holter monitoring) was recently found to be a strong predictor of AF development. Premature atrial contractions (PACs) are positively associated with increasing age, height and B-natriuretic peptide levels and inversely related to HDL and physical activity. PACs have significant prognostic potential that can help identify patients at greatest risk for AF and for whom early intervention may enable primary prevention.
In addition to assessing patients using the Framingham Risk Scoring Method, an evaluation for atrial ectopy should be considered. Patients with risk factors may be treated aggressively and encouraged to take control of lifestyle issues to lower their risk of AF. Although more studies confirming the preventive power of lifestyle changes are needed, primary prevention of AF is less risky than treating it. The fact that current AF therapies are only partially effective and are associated with substantial morbidity and mortality makes the case for primary prevention particularly compelling.
Lifestyle changes may also help prevent recurrent AF. In studies of obese patients who lost weight and experienced resolution of their diabetes as a result of dietary changes and increased exercise, significant differences in the frequency and duration of AF episodes were seen.
Other studies suggest that aggressive lifestyle changes can improve outcomes following endocardial ablation or surgical treatment of AF. Therefore, secondary prevention of recurrent AF should similarly include efforts to optimize weight, control blood pressure and diagnose and treat sleep apnea. Risk-reduction programs for patients before and following AF ablation may have benefits similar to or greater than that of cardiac rehab programs for post-MI patients. Recent studies suggest that lifestyle changes may have a more significant effect than any antiarrhythmic medication.
Preventive lifestyle interventions may have the potential to prevent the development of AF or decrease the burden of AF, while improving overall health and wellbeing. They may also reduce the risks associated with AF, thus lowering the individual and societal costs of managing AF, AF-related stroke and heart failure.
Further studies in larger populations are warranted to confirm and extend this potentially practice-changing conclusion. Nevertheless, your help in recognizing AF risk early—and encouraging lifestyle interventions to address the modifiable risk factors—is needed. The decision for early use of Holter monitoring on an individual may be based on risk-factor burden. By sharing the results of the analysis with the patient, you may empower and motivate them to become more active partners in their own healthcare.

Further acute testing not needed if ECG and high-sensitivity troponin are negative

Scott Cameron, MD, PhD, also brings wide-ranging research interests to bear

Pioneering U.K. vascular surgeon joins Cleveland Clinic

AHA statement is first comprehensive document on perioperative stroke reduction

Recognition reflects prioritization of long-term patient outcomes

Recommendations help distinguish exercise-induced remodeling from pathology

JACC review highlights factors unique to women, ways to tailor management
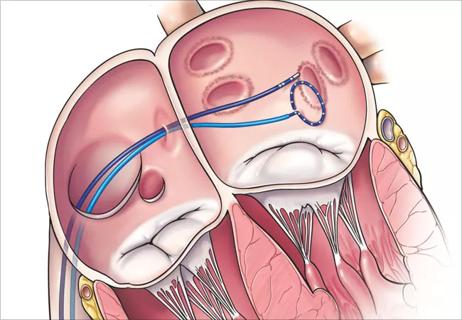
Pushing the envelope in ablation of atrial fibrillation, ventricular tachycardia