Pooling of PARTNER data finds low rates regardless of approach

Prosthetic valve endocarditis (PVE) is comparably rare in both transcatheter (TAVR) and surgical (SAVR) aortic valve replacement, according to a pooled analysis of all PARTNER trials and registries to date.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Despite theoretical concerns about potential inherent infection risk with transfemoral access, we found no elevated risk of PVE with TAVR — whether performed via transfemoral or transthoracic access — relative to SAVR,” says Matthew Summers, MD, a Cleveland Clinic interventional cardiology fellow who presented the analysis at the 2018 Transcatheter Cardiovascular Therapeutics conference (TCT 2018). [Editor’s note: The study was published in full in Circulation on Nov. 6, 2019.]
“While the incidence of PVE following SAVR is well defined in the literature at about 0.3 to 3.0 percent per patient-year in the first year, the corresponding incidence following TAVR is less well characterized,” notes Cleveland Clinic cardiologist Wael Jaber, MD, senior author of the multicenter analysis. “Data on PVE in TAVR are from smaller site-reported registries and are limited to first-generation valves and early TAVR experience. We were pursuing an updated look at this question with data more reflective of current practice and cumulative experience.”
Specifically, the researchers included all 8,285 patients enrolled in the PARTNER I and II trials and the SAPIEN 3 registries. Of these, 7,028 underwent TAVR (84.8 percent) and 1,257 underwent SAVR (15.2 percent). Among TAVR recipients, 70.6 percent had the procedure via transfemoral access and 29.4 percent via transthoracic access. PVE was adjudicated based on modified Duke criteria.
The researchers found a 1.2 percent incidence of PVE over 2.5 ± 1.5 years of follow-up across the entire cohort, which translates to 6.57 cases per 1,000 patient-years.
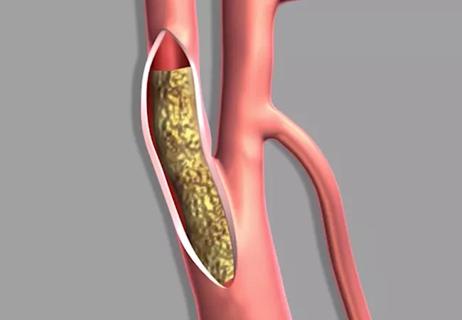
There were no significant differences between the TAVR and SAVR groups in the cumulative incidence of PVE (1.27 percent with TAVR vs. 0.95 percent with SAVR) (see Figure 1) or in the risk of PVE over time out to five years. These results were unchanged by multivariable analyses that controlled for the competing risks of death from other causes (Figure 2).
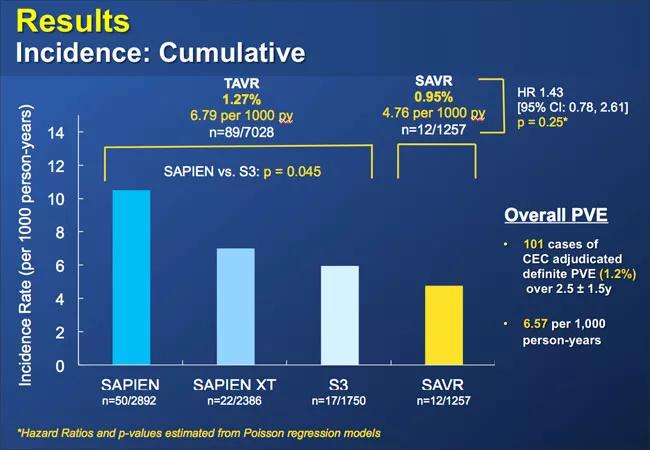
Figure 1
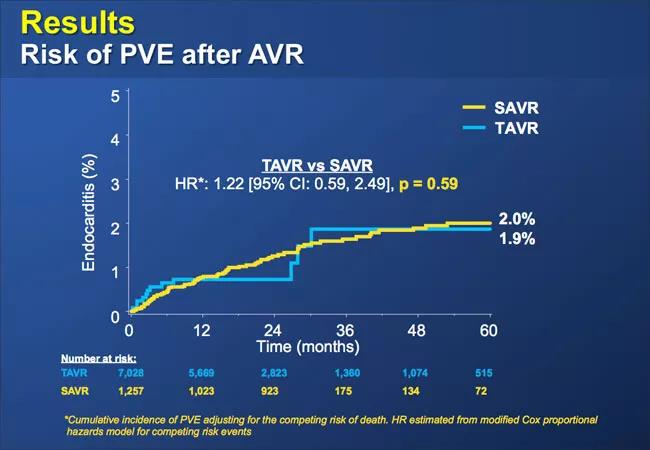
Figure 2
Similarly, the timing of PVE development was statistically comparable between the TAVR and SAVR groups.
The analysis found several patient factors to be significantly associated with PVE:
Notably, transfemoral access for TAVR was not associated with PVE.
When patients with PVE were analyzed by infectious organism, staphylococci were implicated at a significantly higher rate among SAVR patients. The mix of causative organisms was more varied among TAVR recipients, with streptococci involved most often, in nearly a third of cases.
Across both the TAVR and SAVR groups, PVE was associated with a significantly increased risk of death. “Although PVE is a rare event after both TAVR and SAVR, it remains a significant complication with high mortality rates when it does occur,” observes Dr. Jaber, noting that it is an identified mechanism of valve degeneration.
The analysis has several limitations. Because most TAVR cases in the PARTNER trials and registries were performed in the OR with patients under general anesthesia, the TAVR findings may be less applicable to patients exposed to more recent — and more minimalist — TAVR practice. Additionally, despite the inclusion of intermediate-risk patients, the cohort included a higher proportion of inoperable and high-risk patients than may be typical of most current practices.
“Despite these limitations, these findings provide welcome reassurance that the risk of PVE following TAVR is low and highly similar to that following SAVR,” concludes Dr. Summers. “They also give us unique and multicenter insight on PVE with TAVR, as well as a modern report on the incidence and prognosis of PVE with SAVR.”

Surprise findings argue for caution about testosterone use in men at risk for fracture

Findings support emphasis on markers of frailty related to, but not dependent on, age
![GettyImages-1252287413 [Converted]](https://assets.clevelandclinic.org/transform/StoryPanel/350804b2-f1e4-4d97-a277-9629cf45af3e/23-HVI-4120348_redlining_650x450_jpg?w=3840&q=75)
Large database study reveals lingering health consequences of decades-old discrimination
Additional analyses of the two trials presented at 2023 ESC Congress
Prospective SPIRIT-HCM trial demonstrates broad gains over 12-month follow-up

An ACC committee issues recommendations to accelerate sluggish progress
Review of our recent experience shows it’s still a safe option
Machine learning may improve risk prediction and guide therapy