Answer may lie in changes in the tumor microenvironment
Over the past decade, treatment for locally advanced rectal cancer has undergone a paradigm shift. Based on convincing evidence from large randomized controlled trials, the standard of care for locally advanced rectal cancer includes neoadjuvant chemoradiotherapy (nCRT) followed by surgical resection with a total mesorectal excision.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
While this treatment regimen has reduced local recurrence rates to less than five percent in many series, it has had limited effect on overall survival. Distant metastases persist as the principal cause of cancer-related mortality. “There is a pressing need to develop treatments that can prevent this dreaded outcome,” says Cleveland Clinic colorectal surgeron David Liska, MD.
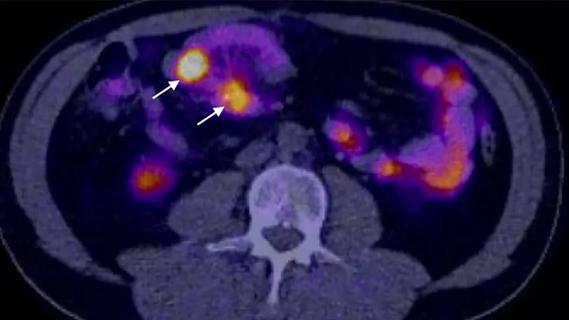
Neoadjuvant CRT changes the pattern of distant recurrence in rectal cancer, with the lungs rather than liver the primary site of metastasis. This may be due to treatment-related alterations in lymphatic drainage or radiation-related changes in the tumor and its microenvironment that preferentially facilitate metastases to certain sites. Recent evidence has established the importance of the cellular microenvironment surrounding epithelial cancer cells, which includes immune cells, vascular endothelia, and, in particular, fibroblasts.
To gain a deeper understanding of nCRT and metastatic rectal cancer, Dr. Liska and fellow researchers Shao Xiang, MD, Matthew Kalady, MD, and Emina Huang, MD, investigated how nCRT impacts cancer progression and metastasis on a molecular level. “We are trying to address how neoadjuvant chemoradiotherapy, particularly radiation, affects tumors and why patients still develop metastatic disease. Since radiation can kill tumors, you would think it would also prevent metastases but neoadjuvant treatment isn’t as effective in reducing the incidence of metastases as it is in preventing local recurrence. So far, most research regarding nCRT has focused on colorectal cancer epithelial cells and no specific gene signature has been identified to help predict which patients will respond to neoadjuvant chemoradiotherapy,” says Dr. Liska.
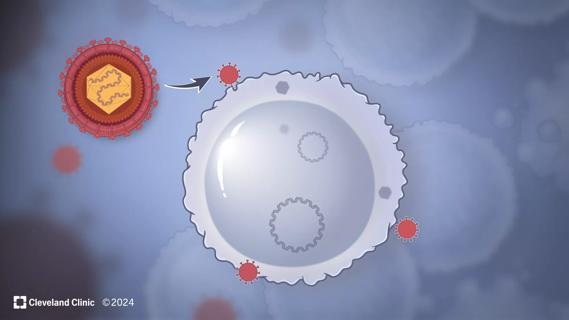
The researchers isolated and propagated primary cancer-associated fibroblasts (CAFs) from rectal cancer patients who had not received nCRT. CAFs are a subpopulation of cells that reside within the tumor microenvironment and encourage tumor growth, angiogenesis, inflammation and metastasis; they also affect the response of colorectal cancer cells to cytotoxic drugs and targeted therapies. Studies have shown that while CAFs survive relatively high doses of radiotherapy, their phenotype is profoundly altered — characterized by growth arrest and a senescent-associated secretory phenotype (SASP). This phenotype leads — in a paracrine fashion — to cancer cell survival and progression.
The primary rectal CAFs were treated with radiation and then harvested and used in experiments that evaluated their effects on in vitro migration and invasion. Also, colorectal cancer (CRC) cells were treated with conditioned media from radiated CAFs and assessed for epithelial-mesenchymal transition (EMT), a developmental program that is increasingly recognized to play key roles in promoting carcinoma invasion and metastasis.
For in vivo work, a novel orthotopic rectal cancer mouse model was used to cultivate primary tumors and metastases which were assessed using in vivo bioluminescence imaging and histologically confirmed.
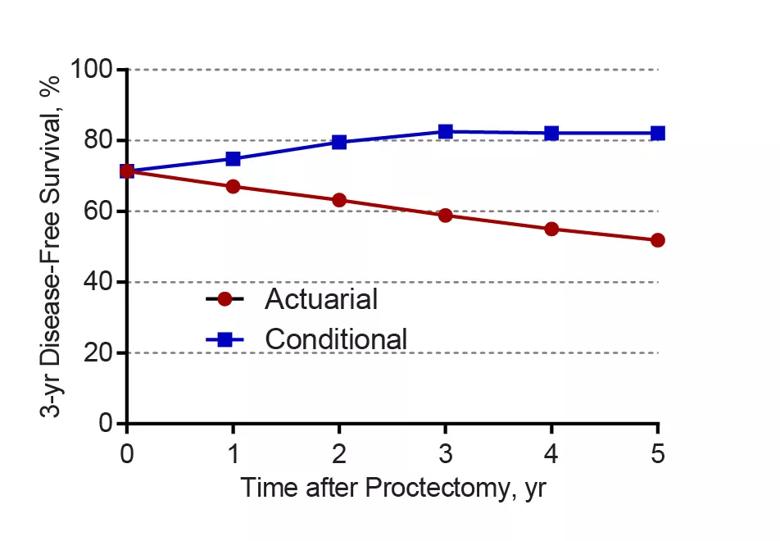
Figure 1. Conditional and actuarial 3-year disease-free survival.
The study is the first to show that radiated CAFs can promote tumor progression in colorectal cancer and how this occurs. Radiated CAFs present in the rectal cancer microenvironment secrete factors that induce EMT in rectal cancer epithelial cells resulting in increased invasion and metastases.
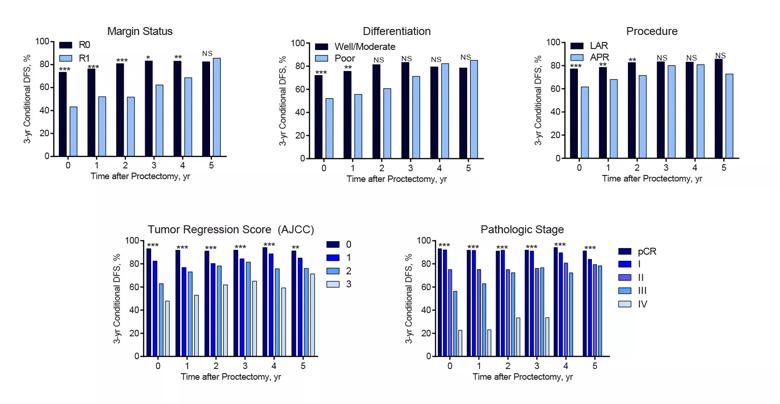
Figure 2. Conditional 3-year disease-free survival stratified by different prognostic factors. LAR, low anterior resection; APR, abdominoperineal resection; pCR, pathologic complete response; *** denotes ppp.
Studies have shown that while CAFs survive relatively high doses of radiotherapy, their phenotype is profoundly altered — characterized by growth arrest and a senescent-associated secretory phenotype (SASP). This phenotype leads — in a paracrine fashion — to cancer cell survival and progression.
The researchers are following up on this study to identify the paracrine factors that control the cellular response to nCRT with a goal of developing drugs that inhibit them. “Once we know which factors increase metastasis, we can develop drugs that reduce metastasis in locally advanced rectal cancer,” says Dr. Liska.
Dr. Liska presented the findings Tuesday at the American Society of Colon and Rectal Surgeons (ASCRS) annual meeting.

An underdiagnosed condition in patients with cancer
Study demonstrates superior visualization of occult primary lesions

New device offers greater tumor control for malignant liver lesions
Cleveland Clinic researchers discover what drives – and what may halt – virus-induced cancer

First-ever U.S. population-level retrospective analysis reveals many patients with systemic mastocytosis need faster intervention

New program provides prehabilitation and rehabilitation services to help patients with cancer maintain and regain function

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients