Exercise, vitamin D and timing

By Luke D. Kim, MD, FACP, CMD Ardeshir Z. Hashmi, MD, FACP
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In 2018, the U.S. Preventive Services Task Force updated its recommendations for preventing falls in community-dwelling older adults. Based on the findings of several trials, the task force recommends exercise interventions for adults age 65 and older who are at increased risk for falls. Gait, balance and functional training were studied in 17 trials, resistance training in 13, flexibility in eight, endurance training in five and tai chi in three, with five studies including general physical activity. Exercise interventions most commonly took place for three sessions per week for 12 months (range two to 42 months).
The task force also recommends against vitamin D supplementation for fall prevention in community-dwelling adults age 65 or older who are not known to have osteoporosis or vitamin D deficiency.
Hospitalized older adults usually spend most of their time in bed. Forty-five previously ambulatory patients (age ≥ 65 without dementia or delirium) in a Veterans Affairs hospital were monitored with wireless accelerometers and were found to spend, on average, 83 percent of the measured hospital stay in bed. Standing or walking time ranged from 0.2 to 21 percent, with a median of only 3 (43 minutes a day).
Since falls with injury became a Centers for Medicare and Medicaid Services nonreimbursable hospital-acquired condition, tension has arisen between promoting mobility and preventing falls. Two studies evaluating the adoption of mobility-restricting approaches such as bed-alarms, “fall-alert” signs, supervision of patients in the bathroom and ensuring patients’ walking aids are within reach, did not find a significant reduction in falls or fall-related injuries.
A clinically significant loss of community mobility is common after hospitalization in older adults. Older adults who developed mobility impairment during hospitalization had a higher risk of death in a large, retrospective study. A large Canadian multisite intervention trial that promoted early mobilization in older patients who were admitted to general medical wards resulted in increased mobilization and significantly shorter hospital stays.
This abridged article originally appeared in Cleveland Clinic Journal of Medicine.
Dr. Kim is staff in the Center for Geriatric Medicine. Dr. Hashmi directs the Center for Geriatric Medicine.

Social prescribing turns leisure activities into good “medicine”

Study highlights importance of responsive, customized approach

Surrogate decision-making appears to increase risk of serious complications

Geriatric Emergency Needs Assessment

Cleveland Clinic joins Yale in new study

Unique model of care helps optimize medications in high-risk cohort
1-Minute Consult: Updated recommendation reflects reduced incidence of disease
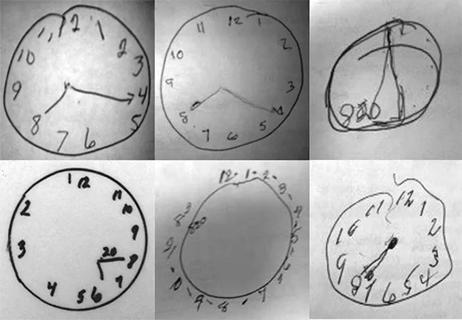
Addressing cognition issues associated with cardiovascular disease