Approximately 5 to 15% of patients undergoing ileal pouch-anal anastomosis (IPAA) for inflammatory bowel disease experience complications leading to pouch failure over their lifetime. Now, an innovative Cleveland Clinic study has found that patients whose pouch survives several years without a complication are likely to have an excellent long-term outcome.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We were able to show the risk is greatest in the first few years. Once patients pass that point, they are likely to have improved chances of keeping their pouch long-term,” says principal investigator Stefan Holubar, MD, MS, Director of Research in Cleveland Clinic’s Department of Colorectal Surgery. “Patients and healthcare providers should find this message reassuring.”
Findings were presented at the 2019 annual scientific meeting of the American College of Colon and Rectal Surgeons by colorectal surgery fellow Adina Feinberg, MD.
Conditional survival is a predictive technique that reveals how survival outcomes are apt to change with the passage of time. Using a modified Kaplan-Meier method, researchers are able to estimate future survival rates when a patient has reached a certain post-treatment time point. The approach has been applied in the oncology setting as a pragmatic way to inform prognosis.
The investigation into conditional IPAA survival was inspired by previous Cleveland Clinic research on the shifting odds of cancer-free survival following surgery and chemoradiation for rectal cancer. In that study, presented at ASCRS 2018, Matthew Kalady, MD, found that survival rates increased as patients passed certain milestones without a recurrence.
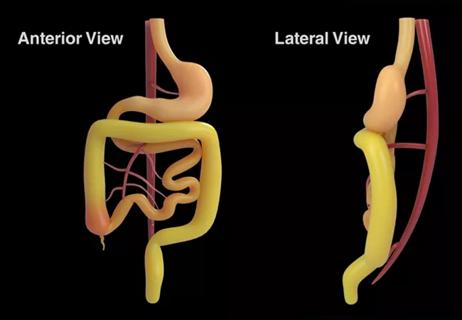
“We thought a similar situation might exist after J-pouch surgery,” says Dr. Holubar.
Risk factors associated with IPAA failure include postoperative anastomotic leak, abscess, fistula and pouch configuration. However, it was unknown whether the importance of these risk factors changed over time.
“We suspected certain risk factors may be associated with an initial risk for pouch loss that decreased with time as the patient gets further out from the acute episode. Conversely, other risk factors might continue to confer the same or greater degree of risk as time progresses,” says Dr. Holubar.
To examine this hypothesis, the researchers queried Cleveland Clinic’s prospectively maintained clinical pouch database to identify patients with ulcerative colitis or indeterminate colitis who had undergone IPAA surgery between 1986 and 2016. After eliminating patients lacking follow-up information, the final sample contained 3,468 patients.
The overall 10-year pouch survival rate was 94%. Conditional pouch survival rates rose to 95% one year post-operatively, 97% after three years and 98% after five years.
The researchers found that in cases with anastomotic leaks or postoperative abscesses, pouch survival improved as the post-complication interval increased. For patients who experienced anastomotic leaks, conditional pouch survival rates increased from 89% after one year to 98% after three years. The researchers found a similar conditional survival pattern for IPAA with postoperative abscesses.
For pouch configuration and fistula, pouch survival rates did not significantly change over time.
“Clinically, this can be explained in that patients with catastrophic infectious complications would be expected to have pouch failure earlier on,” the authors write. “Patients who have salvageable infectious complications which enable them to keep their IPAA for more than a year have a better prognosis in terms of long-term pouch survival. Therefore, as time progresses after the occurrence of an infectious post-operative complication, we observe that the IPAA survival approaches that of patients who did not suffer the complication.”
Patients who are able to heal their presacral sinus (a form of leak) keep their pouches, Dr. Holubar says, while those who do not heal may need a re-do pouch.
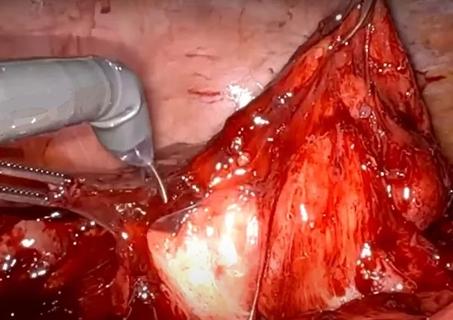
In addition to taking precautionary measures to prevent complications during IPAA surgery, it is incumbent on surgeons to mitigate complications’ effects to the extent possible, says Dr. Holubar. “Newer techniques such as advances in stapler technology, and for managing anastomotic complications, such as vacuum-assisted therapy, may have promise in this respect,” he says.
The lack of significant differences in pouch complications over time associated with pouch configuration and fistula suggest that those events may not be disastrous when they occur early in the postoperative course, although they may be difficult to manage.
“There is some evidence in the literature that the S-pouch may perform worse in the long term, but we didn’t see this,” says Dr. Holubar. “Additionally, there is evidence that early fistulas are associated with leak, and later fistulas are associated with Crohn’s disease, but again, we didn’t see this. Our study suggests fistulas were successfully managed.”
Whether these findings are widely applicable may be determined by pouch configuration, since 91% of patients in the study received a J-pouch, the procedure of choice at Cleveland Clinic for decades.
“We found an overall pouch failure rate of 5%, which is lower than the 10 to 15% reported nationally,” says Dr. Holubar. “Therefore, the results may not be generalizable to all IPAA patients.”
Additionally, the overall rates of pouch failure and risk factors in the cohort were extremely low, possibly underpowering the study’s ability to predict event outcomes.
Nevertheless, this is the first study to apply conditional survival methods to explore risk factors for pouch failure over time. Its implications are encouraging, both clinically and psychologically.
“Patients who suffer anastomotic leak or pelvic abscess but whose pouch survives three years may be counseled that their pouch survival rate is likely to be similar to that of patients who did not have an infectious complication,” says Dr. Holubar.

Technique is useful in patients with diffuse stricturing Crohn’s jejunoileitis

Lifesaving procedure, continued pregnancy and healthy delivery highlight program’s advancement
Robot-assisted technique provides an alternative to open surgery in a complex case

Cleveland Clinic team blends extended mesenteric excision and Kono-S anastomosis

Continued pregnancy and delivery are only the second successful outcome worldwide

FETO and twin-twin transfusion syndrome treatments are next
New procedure eliminates volvulus risk

Measuring outcomes becomes more granular with surgeon-entered data