No evidence of residual tumor or recurrence at 6.5 years of follow-up
By Gene Barnett, MD, MBA, and Manmeet Ahluwalia, MD
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 48-year-old right-handed man presented with recent onset of motor and cognitive dysfunction. He had begun to have vague symptoms of dizziness and unsteadiness about two weeks earlier. Initially these were attributed to a resolving sinus infection, but approximately one week before presentation his wife began to notice more significant cognitive symptoms. He then had an episode of falling while in the shower and was taken to an outside emergency department, where a CT scan revealed a left medial parietal mass. He was placed on dexamethasone and levetiracetam and then sought a second opinion at Cleveland Clinic.
When he was seen at Cleveland Clinic, the patient’s symptoms had resolved and he was neurologically intact. An MRI showed ring enhancement and extensive edema around the mass, which appeared to be situated in the cingulate gyrus, immediately below the left paracentral lobule and the primary motor and sensory fibers (Figure 1).
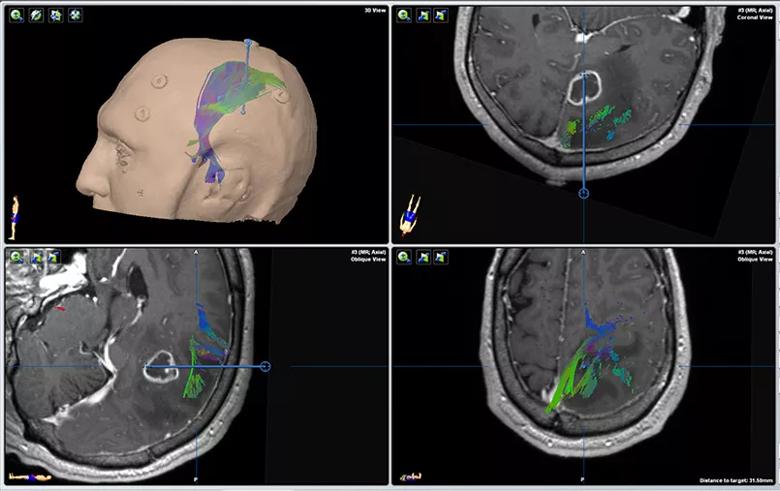
Figure 1. Neuronavigation planning for biopsy and laser ablation showing the relationship of the tumor in the cingulate gyrus to overlying motor and sensory projection fibers and the paracentral lobule. Blue lines indicate the surgical trajectory.
Additional imaging, including diffusion tensor imaging for fiber tracking, was obtained. This led to the determination that any conventional surgical approach (including parafascicular surgery) would subject the patient to a very high risk of motor and/or sensory deficits in his right lower limb because of the sensitive and deep location of the tumor. He was offered stereotactic biopsy and what was at the time — i.e., autumn 2011 — a relatively new therapeutic surgical modality, laser interstitial thermal therapy (LITT), which involves a laser probe only a few millimeters wide.
Five days after his fall in the shower, he underwent the minimally invasive LITT procedure and, as had been predicted, had only mild dorsiflexion weakness of his right foot, which resolved within a few weeks.
The following week, his case was reviewed in one of the twice-weekly multidisciplinary brain tumor boards convened by Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center. The neuropathologist noted that the patient had a WHO grade IV astrocytoma (glioblastoma) without IDH-1 mutation and with a Ki-67 labeling index of 9 to 10 percent and chromosomes 1p- and 19q intact (at that time [2011], the MGMT gene promoter was not routinely assessed). The neuroradiologist confirmed that his postoperative imaging showed a complete ablation of the enhancing portion of the tumor (Figure 2).
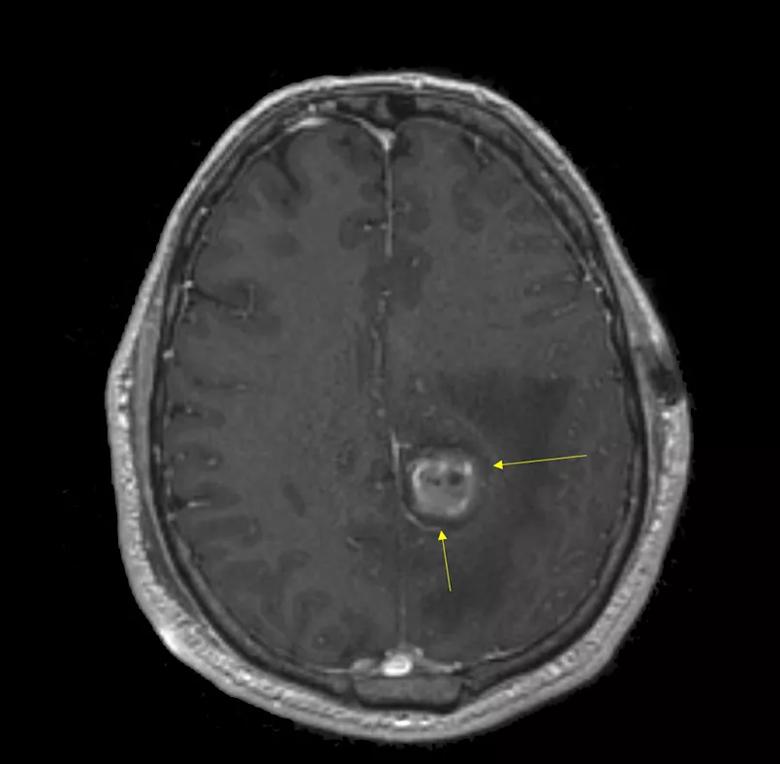
Figure 2. MRI taken 24 hours after ablation showing the extent of ablation (thin eggshell of enhancement indicated by arrows) and loss of contrast enhancement (hyperintensities are post-ablation blood and protein products).
The brain tumor board recommendation was for external beam radiotherapy (60 Gy to the ablation bed + 2 cm) with concurrent temozolomide, followed by high-dose temozolomide for 5 days repeated at 28-day cycles. The patient elected to have the chemo-radiation therapy performed at Cleveland Clinic.
His first imaging after chemo-radiation showed marked improvement in the appearance of the tumor, which was even better at six months (Figure 3). In view of this, his temozolomide therapy was continued for a full year. Serial imaging showed that the tumor remnant continued to decrease, and the patient remained neurologically normal more than six and a half years after his surgery, with no evidence of recurrent or residual tumor (Figure 4).
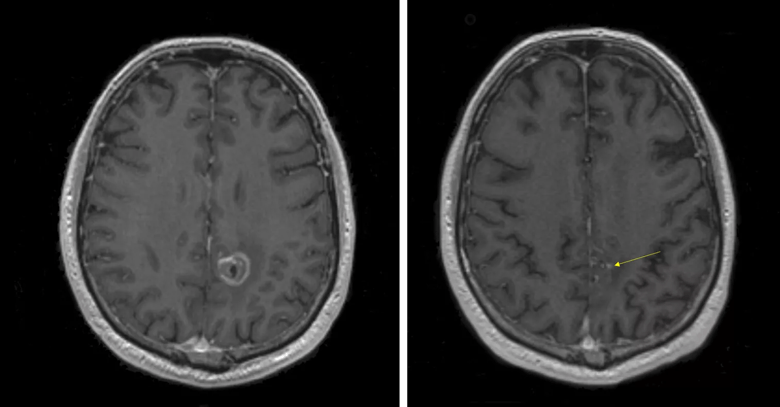
Figure 3 (left). Six-month postoperative MRI with contrast showing decreasing rim of ablation enhancement and overall reduction in lesion size. Figure 4 (right). MRI with contrast taken 6.5 years after ablation showing a single speck of enhancement (arrow) and no clear evidence of residual or recurrent tumor. The patient has remained asymptomatic.
Although stereotactic brain biopsy can provide accurate and safe diagnosis of deep brain lesions owing to the small diameter of the biopsy instrument, it does not provide meaningful cytoreduction of tumor cells. In some cases, a safe corridor can be devised via a minimally invasive craniotomy using neuronavigation (with or without tubular retractors), but the location in this case was not accessible without a high risk of sustained functional morbidity for the patient’s right lower limb. A noninvasive treatment such as stereotactic radiosurgery eliminates the access issue but has been shown not to improve prognosis as part of the initial management of glioblastoma.
LITT (also known as laser ablation) was a relatively new method of minimally invasive cytoreduction at the time of this case in 2011, with the first case of human tumor ablation using this system performed at Cleveland Clinic (by co-author Dr. Gene Barnett) in 2008. Nonetheless, early results in the multicenter clinical trial led by Dr. Barnett — along with subsequent clinical experience after LITT was cleared by the FDA for ablation of brain tissues — were very promising and prompted Dr. Barnett to offer this cutting-edge treatment to the case patient, whose prognosis otherwise looked bleak. Tumor ablation followed by consolidation using a multidisciplinary approach combining chemotherapy and radiotherapy has led to a rare, durable remission of the tumor with no evidence of viable residual tumor or recurrence.
Dr. Barnett is Director of Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center and Professor of Neurological Surgery at Cleveland Clinic Lerner College of Medicine.
Dr. Ahluwalia is the Dean and Diane Miller Family Endowed Chair in Neuro-Oncology in the Burkhardt Brain Tumor and Neuro-Oncology Center as well as Professor of Medicine at Cleveland Clinic Lerner College of Medicine.

An underdiagnosed condition in patients with cancer
Study demonstrates superior visualization of occult primary lesions

New device offers greater tumor control for malignant liver lesions
Cleveland Clinic researchers discover what drives – and what may halt – virus-induced cancer

First-ever U.S. population-level retrospective analysis reveals many patients with systemic mastocytosis need faster intervention

New program provides prehabilitation and rehabilitation services to help patients with cancer maintain and regain function

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients