Mounting evidence argues for operating sooner than now recommended
U.S. and European guidelines give aortic valve (AV) surgery a class I indication in symptomatic patients with aortic regurgitation (AR) and those with depressed left ventricular ejection fraction (LVEF). This is not debated. However, the guidelines give a class II recommendation to pre-emptive AV surgery in asymptomatic patients with preserved LVEF in the setting of a significantly dilated left ventricle. Now a growing body of studies conducted at Cleveland Clinic and validated by others strongly suggest the recommendation to delay AV surgery in asymptomatic patients with AR should be revisited.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The class II recommendations were based on small studies with relatively short-term follow-up from more than two to three decades ago,” says cardiologist Milind Desai, MD, Professor of Medicine at Cleveland Clinic Lerner College of Medicine. “Significant improvements in diagnostic imaging and the emergence of advanced surgical techniques have led to considerable declines in surgical morbidity and mortality. Additionally, the natural history for many asymptomatic patients is no longer as benign, with a mortality of 2.2 percent per year versus the previously reported 0.2 percent per year.”
About five years ago, Dr. Desai and his Cleveland Clinic colleagues developed an interest in the relationship between AV surgery and long-term outcomes in patients with AR, particularly in identifying the threshold of LV dimension at which mortality significantly rises.
“We wondered if we were waiting too long to operate,” he explains. “In primary mitral regurgitation, we operate earlier. Why not in regurgitant AV disease too?”
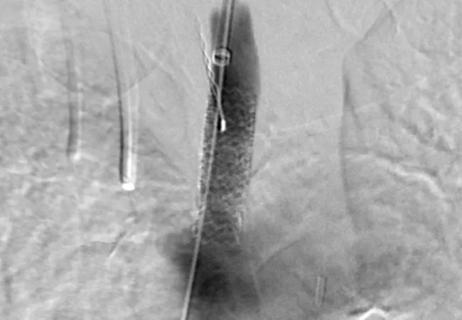
He and colleagues pooled data from 1,417 patients with moderate or severe AR and preserved LVEF seen from 2002 to 2010 at Cleveland Clinic. In this group, 87 percent were asymptomatic. Of the total, 66 percent had undergone AV surgery. The researchers demonstrated that longer-term survival in patients who underwent AV surgery was significantly better than in those who did not undergo AV surgery and was actually similar to that of an age- and gender-matched normal U.S. population sample. The finding was independent of the indexed LV end-systolic dimension (iLVESD) at which patients underwent surgery.
“Furthermore, in the non-operated group, the risk of death significantly and continuously increased once iLVESD exceeded 2 cm/m2, which is a lower LV threshold than previously recommended for surgical intervention in the guidelines,” says Dr. Desai.
These Cleveland Clinic findings were published in late 2016 and recently corroborated in a European study of 356 consecutive patients undergoing AV surgery for severe AR. In this study, adjusted 10-year survival was better among patients with class II indications or without operative triggers than in patients with class I triggers. Similar to the Cleveland Clinic study, this analysis showed that mortality began to rise when LVEF dropped below 55 percent and LVESD rose above 20-22 mm/m2.
When an additional U.S. group recently examined their own population with AR, they reconfirmed the Cleveland Clinic findings by demonstrating, similar to the European study, that waiting for class I indications was associated with worse mortality. In addition, the LV size threshold beyond which mortality increased was demonstrated to be 2 cm/m2, similar to the Cleveland Clinic study finding.
Christine Jellis, MD, PhD, a Cleveland Clinic cardiovascular imaging specialist not involved in Dr. Desai’s research, agrees these collective findings are changing how timing of AV surgery should be approached. “In a center of excellence like Cleveland Clinic, where there is high surgical expertise and success in native aortic valve repair/replacement with very low complication rates, the work by Dr. Desai’s group and others identifies extra incentive for patients to proceed with surgery sooner than guidelines now recommend,” she observes.
These findings, now demonstrated by three separate research groups, suggest an increasing impetus to identify asymptomatic individuals with severe AR and those with early symptoms who are at higher risk for adverse outcomes despite preserved LV function. This requires identifying a better way to grade AR severity.
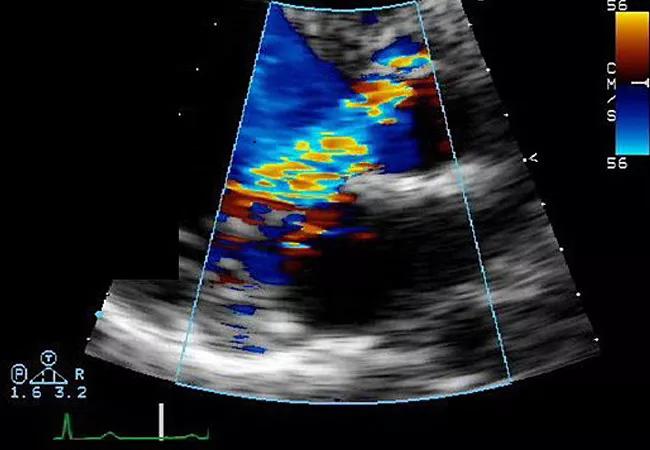
“In echocardiography, we need a multiparametric approach that incorporates LV size and different quantification techniques to better grade the degree of AR,” says Dr. Desai.
He notes that cardiac MRI is increasingly used to quantify AR with emerging incremental prognostic value but questions its current readiness for prime time. “Cardiac MRI techniques need to be standardized and appropriate thresholds developed, while recognizing that the thresholds of severity are likely different than those in echocardiography,” he explains. He adds that more-sensitive markers — beyond LV size, LVEF and aortic regurgitant fraction — are also required for detecting a predisposed individual who would benefit from earlier AV surgery.
In another Cleveland Clinic study of 1,063 asymptomatic patients with severe chronic AR, preserved LVEF and iLVESD < 2.5 cm/m2, Dr. Desai and colleagues found that a LV global longitudinal strain (LV-GLS) worse than –19 percent, measured on transthoracic echocardiography, was associated with lower longer-term survival.
In a newly published follow-up study of 865 patients with severe AR who underwent AV surgery, Dr. Desai and colleagues found that baseline LV-GLS better than –19 percent was independently associated with longer-term survival. They further demonstrated that in the subgroup of patients who returned for follow-up echocardiography 3 to 12 months after AV surgery, 69 percent had impaired LV-GLS (worse than –19 percent) despite their LVEF returning to normal. This subgroup experienced significantly higher longer-term mortality versus those with LV-GLS better than –19 percent. “Worsening of LV-GLS by 5 absolute percentage points from baseline was a cutoff that was significantly associated with longer-term mortality,” notes Dr. Desai.
Dr. Jellis agrees that cardiac MRI and echo strain imaging may become important ancillary tools for determining whether AR is severe enough to warrant surgery. She also underscores the utility of stress echo testing as a complimentary method for stratifying patients for surgery. “Stress echo allows us to evaluate how the heart responds to the additional work required by exercise,” she says. “In some cases of severe AR, an exercise stress test can unmask LV dysfunction that’s not apparent at rest. It also can reveal patients who think they are asymptomatic but actually have poor exercise capacity and have been unconsciously compensating by reducing their activity levels. Those who perform poorly with exercise stress will likely benefit from surgery sooner.”
“From a surgical perspective, we have known for quite a while that asymptomatic patients with chronic AR or mixed valve disease do not recover as well,” adds cardiac surgeon and Cleveland Clinic Heart & Vascular Institute Chair Lars Svensson, MD, PhD, a co-author of Dr. Desai’s studies on this topic. “The new methods of looking at LV strain and MRI evidence of fibrosis will inevitably be included in future guidelines on timing of surgery, as will smaller end-diastolic LV size. Furthermore, if patients in this population are referred earlier for repair instead of replacement, based on recent data we have, surgeons are more likely to be able to repair the valve, as has been found with earlier surgery for mitral valve regurgitation.”
Dr. Desai believes these findings underscore a need to revisit guidelines for surgery for patients with severe chronic AR.
“We should be recommending earlier AV repair or replacement for asymptomatic patients with severe AR and preserved LVEF,” he concludes. “The LV size threshold at which we operate needs to be lower, and we need better techniques for identifying patients who would benefit from earlier AV surgery and for measuring their LV function.”
How our first century has impacted cardiovascular practice

Review offers comprehensive assessment of the landscape for wearables and more

Preserving trust in research requires vigilance and consensus around statistical nuances

Cardiac surgeon Patrick Vargo, MD, reflects on his first year as Cleveland Clinic staff

Improved risk prediction for patients is at the heart of Dr. Aaron Weiss’ research interests

Centralization would likely bring better outcomes, experts say, but may not be feasible
Dr. Daniel Burns on mentorship, robotic valve surgery, statistics and more
JACC review makes the case and outlines how to ensure oversight