Primarily a pediatric phenomenon, co-infection alters the disease course

Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
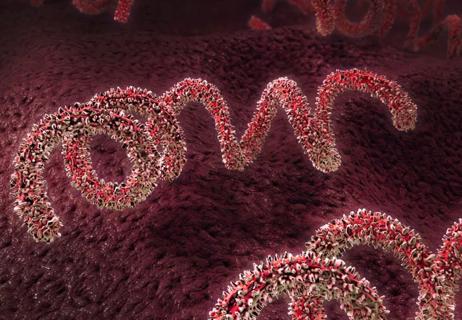
Advancements in multiplex assay platforms have increased our ability to detect numerous respiratory viruses from a single sample. As a result, patients with respiratory tract illness are commonly identified with more than one virus at frequencies as high as 35%.1 Yet, the clinical relevance of mixed viral detections in disease outcomes is unclear.
Studies report that viral co-infections are associated with both increased and decreased severity of disease.2-3 One explanation for the disagreement is an assumption that disease severity associated with co-infection is independent of the pathogen pairings involved. Additionally, mounting evidence suggests virus—virus interactions occur.4 Our understanding of the virus—virus influence between specific viral pairings is piecemeal and incomplete.
We performed a cross-sectional analysis spanning five years of children and adult respiratory viral infections at Cleveland Clinic, which included more than 30,000 respiratory viral panels.5 Of those, nearly 10,000 were positive for any one of 14 different viral pathogens, and more than 1,000 were identified with a virus—virus co-infection.
We set out to determine if, and which, viral species are more predisposed to co-infection and to identify those viral pairings occurring at frequencies different than expected based on co-circulation within the community. Lastly, for those virus co-infection pairings that occur more often than expected, we sought to determine the clinical significance of those pairings.
To do this, we developed a mathematical model to simulate proportional distribution of 66 virus co-infection pairings based on monthly circulation prevalence for each virus within the community. This model provides the expected number of co-infections for each pairing permutation as if no predisposition for any pairing exists, while accounting for both seasonal and year-to-year variation in each viral prevalence. We then identified those pairings occurring at significantly different prevalence than the model’s prediction totals.
While children had more viral infections overall, adults had significantly more positive specimens for influenza (FLU) A and FLUB. Children had substantially more adenovirus (ADV), rhinovirus (hRV), and respiratory syncytial virus (RSV) A and RSVB infections. Viral co-infections are about six times more common in children than adults, with co-infections occurring in 18% of all pediatric specimens compared with only 3% of adult specimens. Co-infections predominated in children under two years of age. Median age of children with co-infection was 13 months, whereas median age in adults was 59 years.
Pediatric patients had substantially higher co-infection rates than adults: 35% of viruses infecting children do so with evidence of a recent concomitant second virus, compared with only about 6% of viruses infecting adults. ADVC had the highest co-infection rate, with 68% of these specimens having at least one additional viral pathogen, while FLUB had the lowest co-infection rate at only 11%. Influenza viruses, along with human metaneumovirus (hMPV) had significantly lower co-infection rates compared to other viral strains. Though rhinovirus had a high co-infection rate in children at 33%, this was not seen in adults (occurring in only 5%) despite being the most common viral infection identified in both age groups and being associated with the most co-infections overall.
This is one of the first studies that analyzes co-infection based on the community circulation patterns of every viral species. Instead of tabulating the numbers as whole over a five-year period, we analyzed the data month-to-month. The result was a much more robust model, which found several viral pairings occurring at much higher prevalence than predicted based on circulation patterns. Several other pairings were notably less likely to occur.
Specifically, three pairings occurred more than predicted by the model: ADVC—hRV, RSVA—hRV and RSVB—hRV. This suggests that these viruses may either directly help each other infect a person simultaneously, or that one virus produces conditions that are beneficial for the second virus to take advantage. Conversely, pairings that were suppressed predominantly occurred between members of the paramyxoviridae family: notably hMPV—Parainfluenza3, hMPV—RSVA and RSVA—RSVB.
Using hospitalization within 48 hours of sample procurement as a broad marker for severity of illness, we found that children who were co-infected with certain pairings had less severe illness than those with mono-infections. This effect was most prominent in the ADVC—hRV pairing; where those children co-infected with both ADVC and hRV were less likely to be hospitalized than those infected with either ADVC or hRV mono-infection.
Our findings suggest that not all respiratory co-infections are random. Certain predilections and aversions appeared between specific viral species. Co-infections are substantially more common in children, especially under two years of age. Specific pairings occur at altered rates than those predicted by proportional distribution, suggesting either direct or indirect interactions result between specific co-pathogens. Additionally, several of these co-infections lead to less hospitalization in children compared to mono-infection. This investigation advances our understanding of co-infection, which may lead to fundamental changes in the interpretation of multiplex respiratory viral screening results and the determination of patient risk for severe disease, while lending important clues to the complex relationships between these important pathogens.
Dr. Esper is Assistant Professor of Pediatrics at Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
Why timely screening and treatment are needed

Collaborative efforts that are shaping best practices

Managing care and counseling your patients

IBAT inhibitors, elastography and more

Programs bring age- and size-appropriate technology to children

Unpacking advancements and identifying drivers of inequity

Self-efficacy mindset, burst therapy and increased biofeedback may help improve outcomes

Pediatric and adult gastroenterologists offer team care for patients with eosinophilic esophagitis