For this multifaceted condition, collaboration in diagnosis and management looms especially large
For patients with trigeminal neuralgia (TN), effective teamwork among different specialists can be critical to optimal diagnosis and treatment, given the condition’s complex presentations, its overlap with other pain syndromes and the variety of possible management approaches.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In fact, multidisciplinary collaboration was an overarching theme of a recent Cleveland Clinic symposium on TN. The symposium — which covered topics ranging from recognizing clinical features of facial and headache syndromes to the importance of diagnostic imaging to pharmacologic, procedural, surgical and psychological treatments — is available free online as 10 video presentations delivered by Cleveland Clinic faculty.
“No single clinician has the experience to optimally deal with this multifaceted disease, which makes collaboration among various specialties essential,” says neurologist Emad Estemalik, MD, Head of Cleveland Clinic’s Section of Headache and Facial Pain and a co-director of the symposium.
Taken together, the symposium’s sessions yielded at least six identifiable ways that providers of neurological care can promote care for TN that is both most appropriate and tends to result in the multidisciplinary teamwork that yields the best results and experience for patients.
“It’s not infrequent that we get referrals for a specific procedure for patients who turn out to have an incorrect diagnosis,” says Varun Kshettry, MD, Surgical Director of Cleveland Clinic’s Trigeminal Neuralgia Program and a co-director of the symposium. “Without conducting our own evaluation, this is a setup for an inappropriate intervention.”
To avoid this problem at Cleveland Clinic, nursing and administrative teams are trained in triaging new patients and referrals to the appropriate specialist for initial contact. “We generally start with an evaluation by a medical expert,” notes Dr. Estemalik. “It is usually not in a patient’s best interest to be advanced to surgical consultation right away.”
Advertisement
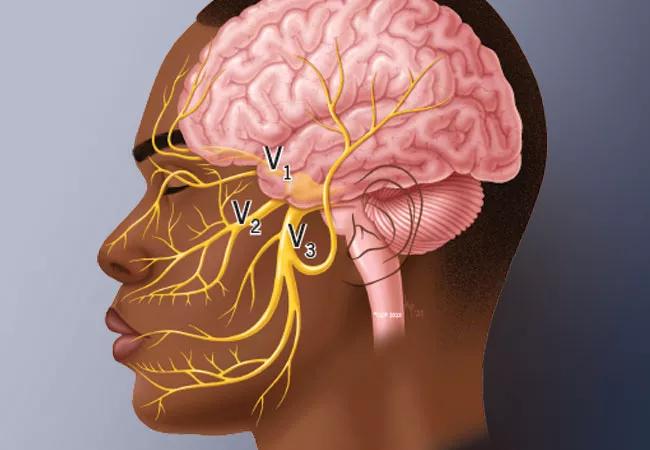
Because no blood test or imaging study can definitively establish the diagnosis of TN, clinical features are key. TN classically presents with episodic, sharp, shooting, burning-like pain within a distribution of the trigeminal nerve, especially the second (maxillary) or third (mandibular) branches. Pain is usually aggravated by talking, chewing or toothbrushing, with patients typically being pain-free between episodes.
It is important to distinguish various headache disorders from facial neuralgias — and to have an understanding of the spectrum of facial pain disorders, Dr. Estemalik explains. In addition to neurological workup, he adds, dental and otolaryngologic causes may also need to be excluded.
When clinical features are consistent with TN, Dr. Estemalik urges further evaluation with sophisticated imaging techniques. “The importance of brain imaging during diagnostic evaluation cannot be stressed enough,” he says. “Not only does it allow detection of nerve compression, indicating the need for advancement to surgical consultation, but it may reveal underlying conditions, such as multiple sclerosis, a primary brain tumor or metastatic brain lesions.”
He and his fellow neurologists in the Section of Headache and Facial Pain draw on the expertise of neuroradiology colleagues to use advanced brain MRI techniques, employing CISS (3D constructive interference in steady state) cuts or FIESTA (fast-imaging employing steady-state acquisition) sequences in addition to MR angiography. These allow detailed evaluation of the trigeminal nerve along its course as well as surrounding blood vessels.
Advertisement
At Cleveland Clinic, optimal patient management is discussed among headache specialists, other neurologists and neurosurgeons.
“The advent of big data and advanced analytics like machine learning and artificial intelligence is improving the ability to predict the chance of pain relief from a surgical procedure,” says Dr. Kshettry. “We often exhaust nonsurgical methods first in patients with a lower predicted chance of pain relief with a procedure, but we will proceed with surgical consultation sooner in patients who have a higher chance of pain relief.”
While most patients respond to initial medical therapy, finding the right drugs that control symptoms with minimal side effects can be a challenge. Anti-seizure medications, skeletal muscle relaxants and antidepressants can be effective options.
Peripheral nerve blocks, sphenopalatine ganglion blocks and botulinum toxin injections are minimally invasive alternatives for patients whose TN is not successfully controlled with medications, especially if they are not good surgical candidates. Off-label therapies can be effective but should be administered by specialists experienced in using them for TN, as techniques and dosages sometimes differ from their use for other conditions.
“There are multiple surgical options for trigeminal neuralgia, and the optimal approach must be chosen with care,” says Dr. Kshettry. Surgical choices, which include microvascular decompression and various rhizotomy procedures, are discussed in a companion Consult QD article here.
Advertisement
Dr. Estemalik advises patients that TN is a chronic condition that can be brought under control but is unlikely to be cured. He often refers them to a colleague trained in discussing functional aspects of chronic pain, such as Taylor Rush, PhD, a Cleveland Clinic psychologist who specializes in chronic pain management and often sees patients with TN.
“The pain of trigeminal neuralgia is often sudden, severe and unpredictable, precipitating a host of behaviors that lead to diminished functioning,” says Dr. Rush, Director of Behavioral Services and Interdisciplinary Programs in the Center for Neurological Restoration. “We can offer many strategies to help patients better cope with their distress.”
She notes that biofeedback — often considered the gold standard for chronic pain management — is not a well-supported technique for facial pain. For patients with TN, she instead emphasizes cognitive behavioral therapy coupled with mindfulness practice to help in regaining a sense of personal control.
Dr. Estemalik offers one final piece of advice to his colleagues in the community: refer patients with suspected TN to a high-volume center.
“Centers like ours have the advantage of seeing enough patients to be able to detect the nuances of different types of facial pain and the potential benefits of the individual therapies for each case,” he says. “For this complex condition, collaboration among specialists with deep experience is important right from the start.”
Advertisement
Advertisement

Swift, aggressive thiamin therapy may be key to preventing long-term neurological injury

Case underscores potential dangers of combining psychedelics with tranylcypromine and stimulant medications

Researchers explore how changes in the gut microbiome influence the brain's reward response to alcohol

Researchers explore new avenues for the management of psychiatric illness in patients with seizure disorders

Addiction experts use decades of research and clinical experience to help patients overcome substance use disorders

Specialized course helps APPs navigate clinical concerns and interpersonal skills

Comprehensive mental health screening may help prevent postsurgical risks

The reassuring potential of psychedelics for the management of substance use and treatment-resistant mental health disorders