The role of interventional pulmonology in cancer care

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0676003e-649d-4305-90fb-316c2a39b065/23-PUL-4190842-CQD-REX-Advanced-Diagnostic-Bronchoscopy-Hero_jpg)
Bronchoscopy
In late 2017, a patient presented to the emergency department with progressive shortness of breath with cough and wheeze. She was known to have chronic obstructive pulmonary disease (COPD), but initial treatment for this COPD exacerbation was not immediately helpful. A CT scan showed evidence of lung cancer invading the trachea and main carina.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cancer invading the main carina is defined as unresectable T4 disease in most cases. She was referred to bronchoscopy for diagnosis and palliation. A rigid bronchoscopy with biopsy was performed to prepare for a stent to palliate the airway. Francisco Almeida, MD, MS, Director of the Interventional Pulmonary Medicine Fellowship at Cleveland Clinic, placed a silicone Y stent, customized onsite to fit the patient, in the trachea. After the stent, she immediately improved and then recovered from her exacerbation. Upon completion of her evaluation, she was found to have Stage IIIB (cT4N2MX) invasive squamous cell carcinoma, moderately differentiated.
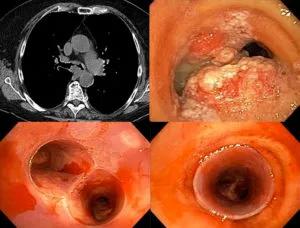
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8135bf76-8828-4383-8e22-34463c3b1aa3/21-CNR-2093458-Inset-1-300x228_jpg)
CT showing irregular mucosa at the main carina (top left). Bronchoscopy showing severe airway involvement (top right). After biopsy and silicone Y-stent bottom airway is widely patent (bottom).
She then underwent concurrent radiotherapy and chemotherapy with carboplatin and paxclitaxel.
After improvement with just two months of therapy and some procedures to manage the stent, a bronchoscopy was performed to determine whether stent removal was possible. Using rigid bronchoscopy, the stent was easily removed.
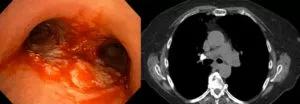
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cef18a31-3310-4c33-930d-9d28f09d36c4/21-CNR-2093458-Inset-2-300x104_jpg)
Although there was evidence of some tumor necrosis, the airway was much improved and the stent was no longer needed (left). CT follow-up imaging showed improvement at the site of the original lesion (right).
In 2020, lung nodules were noted during a surveillance scan. Endobronchial ultrasound, bronchoscopy and biopsy of a peripheral lung lesion were performed. Though the airway showed some evidence of radiation injury, the lymph nodes and lung lesion were nondiagnostic for malignancy. She remains in survivorship and surveillance.
Advertisement
This case highlights the value of multidisciplinary management of malignant central airway occlusion. When faced with critical airway emergencies, interventional pulmonologists can secure and palliate the airway while simultaneously obtaining diagnostic and staging tissue. “And when a patient does need a stent, we can customize it to fit properly, maintain it and then remove it when necessary,” says Thomas R. Gildea, MD, MS.
Cleveland Clinic’s Respiratory Institute has seven American Association of Bronchoscopy and Interventional Pulmonology board-certified physicians making it the largest program in the United States. “We work directly with the interventional pulmonology team on many of our lung cancer patients with airway issues,” says Nathan Pennell, MD, PhD, Director of Cleveland Clinic Cancer Center’s Lung Cancer Program. “It’s an important tool for diagnostics, therapeutics and palliation.”
Research has demonstrated that timely interventions are associated with increased survival and measurable improvements in quality of life and lung function. Recent data from a randomized, controlled trial suggests that early silicone stenting is associated with a more durable palliation of dyspnea and reduced unintended need for bronchoscopy compared with patients who did not receive stents. Further, the EVERMORE study, a multicenter retrospective analysis from Spain, noted that unadjusted Kaplan-Meier estimates showed an increase in one-year survival for patients who received therapeutic bronchoscopy with chemo/radiotherapy compared with chemo/radiotherapy alone (HR = 2.1, 95% CI, 1.1-4.8, P = 0.003).
Advertisement
“We’ve also incorporated patient-specific airway stents into our practice, a process that we developed and that received FDA approval in 2019,” says Dr. Gildea. “Overall, airway stents can play an important role in allowing cancer patients the chance to undergo therapy and to overcome survivorship challenges.”
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches