Minimally invasive, scarless procedures offer more alternatives for patients

Obesity’s complex etiology and its nature as a chronic, relapsing disease necessitate a multispecialty approach to management.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dietary and lifestyle modification, pharmacotherapy and bariatric surgery have been the traditional mainstays of comprehensive obesity treatment programs. Each modality has potential benefits and limitations, and none by itself is universally applicable to patients struggling with obesity. Bariatric surgery is the most effective intervention for weight loss, but less than 1% of eligible patients undergo bariatric procedures annually. Even in the most successful bariatric programs, some patients may regain weight postoperatively, which illustrates the importance of longitudinal care and close follow up.
In the last decade, bariatric endoscopy has emerged as an additional therapeutic option, helping fill the gap between medical treatment and bariatric surgery.
Cleveland Clinic recently has begun a bariatric endoscopy program that is integrated into the institution’s overall multispecialty bariatric weight loss initiatives. The program provides a comprehensive range of endoscopic procedures to address various needs: as primary therapies for patients with obesity; as secondary treatment when patients have regained weight after bariatric surgery; and to address complications stemming from bariatric surgery.
“Not all patients have the same needs,” says newly appointed Director of Bariatric Endoscopy Roberto Simons-Linares, MD. “Bariatric endoscopy is in a kind of sweet spot in terms of invasiveness and efficacy. With its addition at Cleveland Clinic, we have an even greater variety of programs and options available for patients.”
Advertisement
Obesity — defined as a body mass index (BMI) of 30 or higher — is a common, serious and costly disease that affects nearly half of all adults in the United States, according to the Centers for Disease Control and Prevention. It is associated with significant health risks, including heart and kidney disease, stroke, diabetes and certain cancers. Obesity disproportionately affects black and Hispanic adults and people with fewer economic resources.
Traditional bariatric surgery is considered an appropriate option for patients with Class 2 obesity (BMI of 35 to < 40) and comorbidities, and for any patients with Class 3 or severe obesity (BMI > 40). Until the advent of bariatric endoscopy, patients who did not qualify for or did not want to undergo weight-loss surgery were limited to pharmacotherapy and lifestyle/dietary modification as primary treatment.
Primary bariatric endoscopy procedures include:
Advertisement
Dr. Simons-Linares and other members of the multidisciplinary obesity care team work together to determine whether endoscopy or another approach is the most suitable primary treatment for a patient with obesity, while taking the patient’s preferences into account and providing personalized care.
“We collaborate closely with our bariatric surgery partners as well as specialists in obesity medicine, endocrinology, cardiovascular disease, hypertension and sleep medicine, among others,” he says. “Sometimes bariatric endoscopy is the best option, and other times a patient is better served with a surgical gastric bypass and I will refer them to my colleagues. The whole point is doing what’s best for the individual patient.”
Bariatric endoscopy may also serve as an interim treatment for patients who need to lose weight to qualify for surgeries such as joint replacement or organ transplant, and as a means for patients with obesity who have recovered from cancer to lose weight, improve their health and reduce the risk of cancer recurrence.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3848c09e-15eb-4f3d-8db9-f15937f6d828/21-DDI-2191234-Bariatric-balloon-800x550-1-150x113_jpg)
Intragastric balloon.
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/83727539-77ad-43fb-a000-64de41896265/21-DDI-2191234-Bariatric_Mucosal-Ablation-800x550-1-150x135_jpg)
Mucosal ablation.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dca3bef5-2368-471c-9141-d35adf5df80f/21-DDI-2191234-Bariatric_Endobarrier-800x550-1-150x120_jpg)
Duodenal liner.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/05da2a78-a7dc-47f4-a5c5-f3b0813a7873/21-DDI-2191234-Bariatric_Aspiration-Therapy-800x550-1-150x103_jpg)
Aspiration therapy.
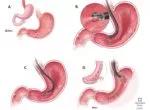
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8874f731-33a9-41a8-b598-757dd433f3c4/21-DDI-2191234-Bariatric-ESG-800x550-1-150x110_jpg)
Endoscopic sleeve gastroplasty.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9ca1c5b2-fbd1-499d-8032-92b8ed257764/21-DDI-2191234-Bariatric-TORe-procedure-800x550-1-150x107_jpg)
Transoral outlet reduction (TORe).
While traditional bariatric surgery to create a restricted or malabsorptive anatomy can produce substantial initial weight loss and improve comorbidities such as diabetes and hypertension, some patients may regain weight postoperatively.
The etiology of postoperative weight regain is complex, but may sometimes be due in part to eventual dilatation of the gastrojejunostomy or expansion of the gastric pouch in gastric bypass patients or dilation (stretching) of the gastric sleeve anatomy in sleeve patients. There are several minimally invasive endoluminal procedures that are effective alternatives to surgical revision for regained weight, including:
Advertisement
Endoscopy also can be useful to assess and manage complications resulting from surgery, including:
Since the program’s launch in August 2021, Dr. Simons-Linares and his team have utilized bariatric endoscopy for all types of obesity treatment: primary, secondary and to address postsurgical complications.
Dr. Simons-Linares received his bariatric endoscopy training in a dedicated fellowship at Boston’s Brigham and Women’s Hospital, Harvard Medical School, under the tutelage of Christopher Thompson, MD, one of the pioneers of the field. Specialized training from experienced teachers at a high-volume bariatric treatment center is essential for good outcomes, especially in complex cases, he says.
“Our program at Cleveland Clinic provides the full spectrum of bariatric endoscopy,” Dr. Simons-Linares says. “We benefit from the large volume of bariatric surgery patients and patients with obesity that we treat. As our bariatric endoscopy program grows over the next year or two, I don’t see any barrier to starting our own bariatric endoscopy fellowship to train future experts in these advanced bariatric procedures.”
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications