Results from an artificial intelligence model

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Over 1 million people in North America live with Crohn’s disease (CD) and nearly 25% are diagnosed before 20 years of age.1 Patients with pediatric-onset CD endure a lifelong disease burden with high rates of disease progression, increased risk of recurrent surgery and decreased height potential.2
Over the past two decades, there has been a paradigm shift in the treatment of CD with the development of biologic agents.3,4 While biologics have shown to improve short-term outcomes, it has been difficult to show the long-term benefit of biologic therapy from standard trials. A team of clinicians, statisticians and computer analysts have come together to answer this question.
Cleveland Clinic is uniquely positioned to study CD as most patients transition from pediatric to adult gastroenterology physicians within the same hospital system and electronic medical record (EMR). This allows for robust evaluation of outcomes and a better understanding of the natural history of a disease. Starting with an EMR database of over 3.5 million patients, we screened patients from 2000 to 2017 using ICD codes to identify 4,815 patients with possible CD. This was followed by a physician chart review in which 51.7% of 300 selected children were confirmed to have CD by myself and adult IBD expert Jean-Paul Achkar, MD.
A model was then constructed of predictors of CD by a team of statisticians led by Michael Kattan, PhD, Chair of Quantitative Health Sciences. His team used natural language processing (NLP) to detect key terms identified by myself and Dr. Achkar on millions of notes from possible patients. NLP is a type of artificial intelligence that allows for analysis of vast amounts of unclassified data in physician, endoscopy, operative, imaging and pathology reports. NLP terms along with discreet data such as ICD codes or procedure codes were then combined into a model to predict an established diagnosis of pediatric-onset CD in 2,060 with a positive predictive valuate of 98.5%. In combination with 4,973 adult-onset CD, the final set of 7,033 CD patients is the largest single center CD cohort in North America.5
Advertisement
The first biologic, infliximab, was approved by the FDA in 2007 for pediatric CD. It has been difficult to demonstrate the long-term benefits of biologic therapy. In our study, we found biologic to exposure after diagnosis was 27.2% at 1-year, 61.8% at 5-years, and 82.2% at 10 years (Figure 1).
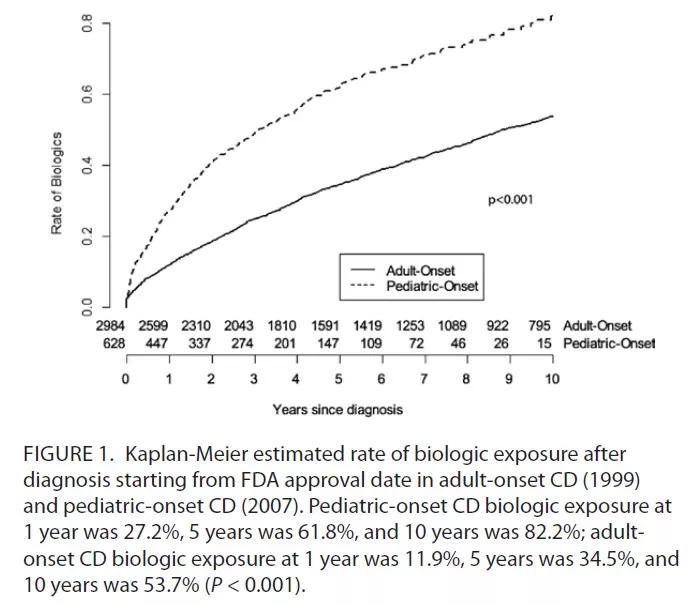
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e17c41d0-c636-4556-86e6-617c71aa253a/Kurowski_Figure-1-2_jpg)
Reproduced with permission from Oxford University Press. Kurowski JA, Milinovich A, Ji X, et al. Differences in Biologic Utilization and Surgery Rates in Pediatric and Adult Crohn’s Disease: Results From a Large Electronic Medical Record-derived Cohort. Inflamm Bowel Dis. 2021;27(7):1035-1044. doi:10.1093/ibd/izaa239
We then found a significantly lower rate of abdominal surgery in those who received six months or more of biologic therapy compared to less than six months (39.1% vs 64.1%, P < 0.001). Further, we reported a significantly lower rate of CD-related abdominal surgery (Kaplan-Meier estimated risk) at 10 years after diagnosis of 43.1% if diagnosed before 2007 compared to 25.5% if diagnosed after 2007 (P < 0.001) (Figure 2).
In addition, we did not find any difference in the rate of high-risk features including intestinal stricture, intra-abdominal fistula or perianal abscess between the two groups. The presence of previous perianal surgery was a significant risk factor for CD-related abdominal surgery (Hazard Ratio 1.74, 95% CI 1.52-1.99, P < 0.001).
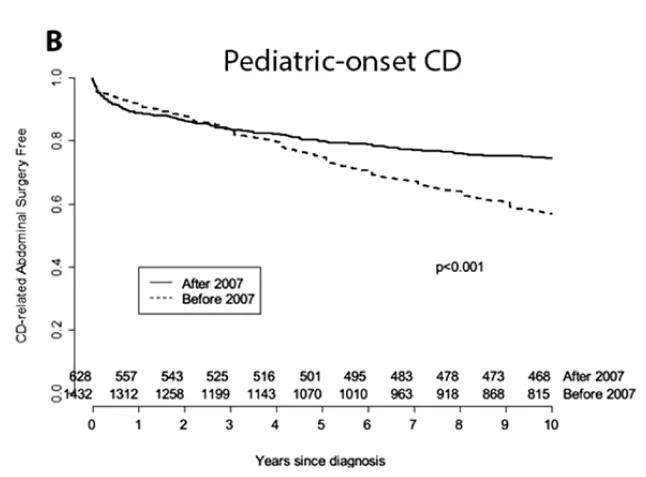
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e5f8394b-8b97-41c4-bfce-5b81fde2e6f9/Kuroswki_2_jpg)
Figure 2. Reproduced with permission from Oxford University Press. Kurowski JA, Milinovich A, Ji X, et al. Differences in Biologic Utilization and Surgery Rates in Pediatric and Adult Crohn’s Disease: Results From a Large Electronic Medical Record-derived Cohort. Inflamm Bowel Dis. 2021;27(7):1035-1044. doi:10.1093/ibd/izaa239
Advertisement
NLP opens up the door to a detailed analysis of complex pediatric diseases, including both common and rare complications. Identification of modifiable risk factors potentially allows for reduction of complications and increases patient-specific disease interventions.
References
About the author: Dr. Kurowski is a pediatric gastroenterologist at Cleveland Clinic Children’s and Assistant Professor of Pediatrics, Cleveland Clinic Lerner College of Medicine at Case Western Reserve University.
Advertisement
Advertisement

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve