Training, resources help with meaningful palliative care conversations

When it comes to end-of-life conversations, patients may expect their doctors to take the lead, yet physicians often feel unsure about doing so. Specialized communication skills can improve the experience for patients and caregivers, says Laura Shoemaker, DO, MS, FAAHPM, Chair of the Department of Palliative and Supportive Care at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Specialty palliative care offers uplifting support for people living with serious illness in order to improve quality of life — whether emotional or physical. Palliative care specialists provide an extra layer of support by working with a patient’s other healthcare teams to provide care alongside curative treatment at any age and at any stage in the course of a serious illness.
Dr. Shoemaker has dedicated her professional life to decreasing the suffering related to the effects of serious illness on patients, families and fellow caregivers. She navigates the symptomatic and practical caregiving needs and is buoyed by the work that she does. “It’s about doing work that’s deeply meaningful and connected to the reason we came to healthcare – doing work that’s connected to our ‘why,’” says Dr. Shoemaker.
“It would be very difficult for me to do my day’s work if I didn’t feel impact or meaning,” she says. “Even after I’ve had a heartfelt discussion with a family or a patient about dying or end of life, if I’ve helped them relieve their anxiety or can help align the medical interventions with their goals and preferences, then I feel satisfied. Even though the experience is sad, it’s actually extraordinarily life affirming.”
Palliative care educators teach clinicians to explore the patient’s perspective before offering advice to best support the patient and family in their decision making. “In my experience, telling doesn’t work as well when we are talking about a serious illness,” Dr. Shoemaker says. “We need to move away from telling and move more toward asking.”
Advertisement
Dr. Shoemaker starts the conversation with questions for the patient: What is their understanding of what is happening with their health? What have other care providers shared about their disease? Where you they in the trajectory of the disease? What treatment options have been offered so far? What are their hopes, worries and fears?
“Before I can even begin to think about recommendations — the ‘telling’ part of medicine — there has to be a conversation so that we can contextualize and better understand the patient’s family values, their preferences and their goals,” Dr. Shoemaker says. “I can’t begin to say where we should go next until I understand more and probe with more questions.
About halfway through an appointment, Dr. Shoemaker sometimes stops to acknowledge to the patient that she has asked many questions, and to reassure the patient that she will be sharing recommendations.
Dr. Shoemaker acquired advanced communications skills during a yearlong palliative medicine specialty fellowship and by continuing to learn as she practices.
To begin to set the stage for a conversation, she recommends viewing resources from The Conversation Project website. Download Your Conversation Starter Kit, which patients and practitioners can use to reflect on, discuss and describe one’s personal values for end-of-life care. It is an initiative of the non-profit Institute for Healthcare Improvement.
Another resource for providers is the Center for Advanced Palliative Care (CAPC), a network of health care professionals from more than 1,700 organizations. The site contains essential tools, training and technical assistance for all clinicians caring for people with a serious illness.
Advertisement
For patient-facing resources, or to identify palliative care programs in your community, GetPalliativeCare.org offers a USA provider locator. The website is provided by CAPC.
Advanced Communications – Making It Foundational
In 1987, Cleveland Clinic established one of the first palliative care programs in the country. The first physician training program for palliative care was built in the 1990s before it was identified as a specialty. Today’s providers receive advanced communications training through the Center for Excellence in Healthcare Communications, Office of Patient Experience.
Smaller organizations that lack a specialty palliative care infrastructure can still benefit from understanding best practices, and may find it helpful to start by identifying palliative care champions and offering education on primary palliative care competencies to a wide range of caregivers.
Dr. Shoemaker underscores the value of awareness.
“It’s all about communications and making sure when someone consults us, we work very closely with all members of the medical team to ensure relationship-centered care. When we sit down with patients and families, it’s about listening a whole lot more than about telling. It’s incredibly life affirming. The focus is on life, not just death.”
For more information on Cleveland Clinic Global Executive Education contact the team online at clevelandclinic.org/execed.
Advertisement
Advertisement

Advanced software streamlines charting, supports deeper patient connections

How holding simulations in clinical settings can improve workflow and identify latent operational threats

Interactive Zen Quest experience helps promote relaxing behaviors

Cleveland Clinic and IBM leaders share insights, concerns, optimism about impacts
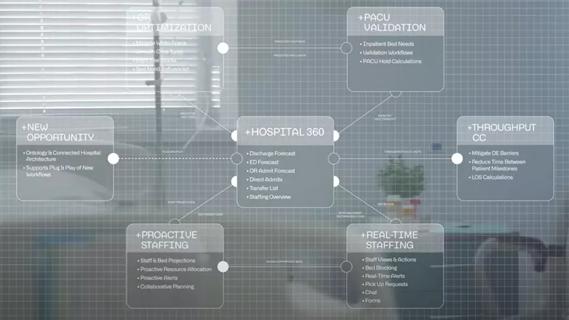
Cleveland Clinic partners with Palantir to create logistical command center

A Q&A with organizational development researcher Gina Thoebes

Cleveland Clinic transformation leader led development of benchmarking tool with NAHQ

Raed Dweik, MD, on change management and the importance of communication