For patients with kidney disease, failure to recognize all parathyroid glands can result in failed surgery

A 29-year-old woman presented to Cleveland Clinic with persistent tertiary hyperparathyroidism. The patient was born with congenital nephrotic syndrome and underwent kidney transplant at age 9, followed by eventual rejection and peritoneal dialysis. In 2018, the patient underwent a repeat kidney transplant.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient had also previously undergone two parathyroid surgeries at other medical centers prior to consulting with physicians at Cleveland Clinic. The first surgery was performed more than 20 years prior to her coming to Cleveland Clinic and was a subtotal parathyroidectomy. The right upper parathyroid was removed along with the right lower parathyroid, left upper parathyroid gland and a portion of the left lower parathyroid.
The patient’s second surgery was in July, 2020, and her surgeon removed a portion of the left lower parathyroid remnant. Intraoperative parathyroid (IoPTH) level was 206 at the beginning of the operation and 270 at the end of the operation. Her calcium and parathyroid hormone (PTH) levels remained high post-operatively.
The patient was told that she was not a surgical candidate, and she was placed back on cinacalcet to help lower calcium levels. At this point, she was evaluated by Brian Stephany, MD, a nephrologist at Cleveland Clinic, who referred her to Cleveland Clinic’s Endocrine Surgery Department for surgical treatment of persistent tertiary hyperparathyroidism.
When she presented to Cleveland Clinic’s Endocrinology & Metabolism Institute, her creatinine ranged from 1.5 – 2.5 mg/dL. Biopsy of the transplanted kidney shows calcinosis due to hyperparathyroidism. The patient met with Katherine Heiden, MD, an endocrine surgeon in Cleveland Clinic’s Endocrinology & Metabolism Institute. At the time of initial evaluation, the patient had the following levels: Ca at 10.9 mg/dL, PTH at 201 pg/mL, creatinine at 2.4 μmol/L, and vitamin D at 25-OH 31 ng/mL. A Sestamibi scan performed after the patient’s second parathyroidectomy suggested an overactive parathyroid in the left posterior neck, and an outside ultrasound revealed a 1.2 cm left thyroid nodule.
Advertisement
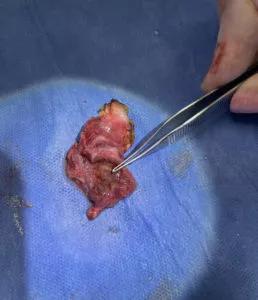
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/335057d6-633c-4110-bdff-8368d8c29f4e/21-EMI-2377213-CQD-Inset-800x930-1-258x300_jpg)
Left thyroid gland with forceps pointing to an enlarged parathyroid gland completely within the parenchyma of the thyroid gland.
Ultrasound was performed in the office during her initial visit with Dr. Heiden. It revealed a hypoechoic structure measuring 1 x 0.8 x 1.4 cm in the left thyroid. The structure had the appearance of a thyroid nodule versus an intrathyroidal parathyroid. Results of fine needle aspiration (FNA) showed cells of parathyroid origin, and PTH level from aspirate was 6,512 pg/mL, confirming that it was a supernumerary intrathyroidal parathyroid gland. In addition, a hypoechoic structure measuring 0.7 x 0.9 x 1 cm was also visualized in the left lower neck with typical appearance of enlarged parathyroid gland. This corresponded to the known parathyroid remnant.
Based on the findings, it was determined that the best course of action was surgery. The patient underwent successful left thyroid lobectomy with en bloc removal of intrathyroidal parathyroid gland. In addition, the left lower parathyroid remnant appeared hypertrophied, so Dr. Heiden elected to resect the remnant and re-implant a portion of the tissue into her strap muscles. The remainder of the remnant parathyroid tissue was cryopreserved. The patient’s IoPTH level decreased from 1,696 at the beginning of the surgery to 82 at the end of the surgery. The patient’s serum calcium levels have remained normal since surgery.
When treating patients with hyperparathyroidism, in particular hyperparathyroidism caused by kidney disease, it’s important to remember that patients can have more than four parathyroid glands. “Failure to recognize this can result in failed surgery, which is what happened twice in this patient’s case,” explains Dr. Heiden. “Once this patient’s intrathyroidal parathyroid gland was removed, she responded well and her calcium levels normalized. This is critical for her overall health as well as for survival of her transplanted kidney.”
Advertisement
It’s also important to note that occasionally parathyroids can be difficult to identify with imaging alone. When they are located within thyroid gland itself, they can mimic thyroid nodules, so Dr. Heiden recommends using pre-operative FNA to help distinguish thyroid nodules from intrathyroidal parathyroid glands. The aspirated fluid can be evaluated for PTH levels to help identify any structures in question. For serum levels, the normal range for PTH is typically 15 – 65 pg/mL (some times as high as 85 pg/mL depending on the lab). For levels in an aspirate, a level close to serum PTH value in a nodule that is not a parathyroid gland versus a very high level (often >1,000) would be expected in an intrathyroidal parathyroid.
Advertisement
Advertisement

Pheochromocytoma case underscores the value in considering atypical presentations

Advocacy group underscores need for multidisciplinary expertise

A reconcilable divorce

A review of the latest evidence about purported side effects

High-volume surgery center can make a difference

Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D

Patients spent less time in the hospital and no tumors were missed

A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications