A brief look at our programs
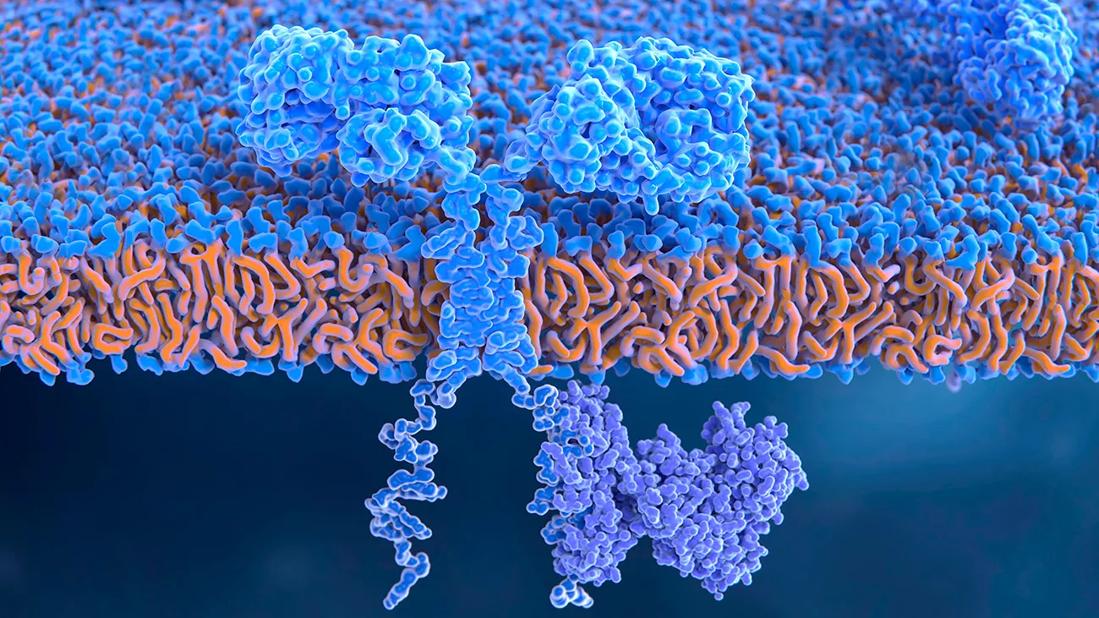
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3984d9a0-25c8-4afd-92f2-fa6a7e6278da/2066588-1300X900_jpg)
Chimeric antigen receptor on T-cell, illustration
In recent years, the momentum created by the initial effectiveness of chimeric antigen receptor (CAR) T-cell therapy has prompted team-based research efforts in cellular therapy at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Learn more about a few of our efforts:
Preliminary data from a phase 1 trial of allogeneic CAR T-cell therapy shows therapeutic responses in relapsed/refractory multiple myeloma (RRMM) patients. In the UNIVERSAL trial, a multicenter study which includes Cleveland Clinic, patients are first treated with a lymphodepleting regimen of cyclophosphamide, fludarabine and ALLO-647, an anti-CD52 monoclonal antibody. Following ALLO-647, they are treated with the CAR T-cell therapy, ALLO-715, which targets BCMA. BCMA is highly expressed on plasma and multiple myeloma cells.
The trial is testing ALLO-715 as a single infusion across four doses: 40, 160, 320, or 480 x 106 CARs. Lymphodepletion regimens consist of fludarabine (F; 30 mg/m2/day) plus cyclophosphamide (C; 300 mg/m2/day) given on three days with ALLO-647 (A; 13-30 mg x 3 days; FCA) or cyclophosphamide plus ALLO-647 (CA).
The therapy generated the strongest response in patients who received ALLO-647 at 320 x106. For this cohort, the overall response rate (ORR) was 60% among 10 patients, including three of six who received CARs with low–ALLO-647 FCA and three of four who had the therapy with high–ALLO-647 FCA. Overall, six patients had a very good partial-plus response (VGPR+), a complete response or a very good partial response (VGPR). This included one patient at 160, four patients at 320 and one at 480 10 x 106 CARs. Of the VGPR+ patients, five were negative for measurable residual disease.
Additionally, six of nine patients treated at the 320 or 480 x 106 dose levels remain in response. Cleveland Clinic has one patient in the trial who has had a good response so far.
Advertisement
“We currently don’t have good therapies for patients who have been treated with three or more prior therapies. CAR T-cell therapy could be a good option for relapsed patients who don’t have the option of waiting,” says Faiz Anwer, MD, staff, Department of Hematology and Medical Oncology, Cleveland Clinic Cancer Center.
Read more here.
Built upon foundational work at the National Cancer Institute (NCI), Cleveland Clinic studies are in development to explore the use of autologous tumor-infiltrating lymphocytes (TILs) and natural killer (NK) cells to produce durable, complete responses for patients with refractory disease.
“Our main focus in melanoma is on recapitulating what has been done by NCI, and we are working with commercial companies to scale up TIL therapies,” says Brian Gastman, MD, Medical and Surgical Director, Melanoma and High-Risk Skin Cancer Program. “We want to make these treatments available to our patients as soon as possible, if not as a potential cure, then as a bridge to other therapies that may be developed in the future.”
In Merkel cell carcinoma (MCC), researchers are testing the expansion of NK cells. In a recent phase 2 trial, treatment with the TIL therapy known as lifileucel produced an overall response rate (ORR) of 36.4% and a disease control rate of 80.3% in patients with metastatic melanoma. The participants had a high baseline disease burden and disease that had progressed on multiple prior therapies, including anti-PD-1 and BRAF/MEK inhibitors.
Advertisement
“This therapy is not standard of care yet and is offered to patients in clinical trials as fifth- or sixth-line treatment,” says Dr. Gastman. “Our hope would be to use TILs earlier to get more benefit, but even for late-stage melanoma, it represents a new option that we may soon be able to give to patients.”
While two trials of TILs for melanoma supported by Cleveland Clinic are still on the drawing board, one with NK cells in MCC is already recruiting. The phase 2, single-arm study will evaluate the immunotherapy in combination with the PD-L1 monoclonal antibody avelumab and the IL-15 agonist N-803.
“The cell therapy product we’re studying for MCC combines modern immunotherapies with reinvigorating therapies,” says Dr. Gastman. “The NK cell line has been engineered to produce endogenous, intracellularly retained IL-2 and to express CD16.”
Unlike TILs, which target antigens in a tumor and are autologous, the NK cells target proteins and are allogeneic products. Both protocols, however, are complex, requiring specialized expertise and careful coordination of patient care at multiple steps.
“Administration of these immunotherapies is complicated,” says Dr. Gastman, “and particularly when lymphodepletion is needed, because of the potential for major side effects, we work closely not only with medical oncologists but also with Cleveland Clinic’s bone marrow transplantation team, which has tremendous experience.”
Read more here.
Betty Hamilton, MD, Associate Director, Blood and Marrow Transplant Program, is working to help coordinate and operationalize novel cellular therapies within different cancer programs across Cleveland Clinic Cancer Center to support participation in and expansion of new clinical trials.
Advertisement
Cleveland Clinic’s Cellular Therapy Assist Team (CAT), housed within the Blood and Marrow Transplant (BMT) program, supports cellular therapy program research groups, such as myeloma, leukemia, thoracic oncology and melanoma, in understanding how to manage cell therapy trials and resources.
The team consists of physicians, research coordinators, nursing and program managers. Team members discuss the logistics and operations of cellular therapy collection and administration within clinical research trials. The group also reviews the portfolio of studies and opportunities for new research and expansion while collaborating between disease groups.
“We’ve created a successful model for collaborative research and experience in cellular therapy among different disease groups,” says Dr. Hamilton. Since CAT’s inception, six new cell therapy studies have been added to Cleveland Clinic’s research portfolio in five months. There are:
Read more here.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches