A look at EDGE, TIF and endoscopic fistulotomy
The emergence of endoscopy has created many opportunities for shorter, safer procedures for common gastrointestinal (GI) conditions that in the past typically were treated surgically or medically. Here are three procedures that Cleveland Clinic is now offering:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In order to access the excluded (stapled off) portion of the stomach and the opening of the bile duct and pancreas in patients who have undergone gastric bypass surgery and now have pancreatic and/or bile duct problems, an endoscopist and surgeon must often work together: The surgeon makes an incision in the belly and brings the stomach closer to the abdominal wall, and then makes an incision in the stomach into which the endoscopist inserts the endoscope and can then reach the ampulla. This technique is difficult to perform and typically requires a one- to two-day hospital stay.
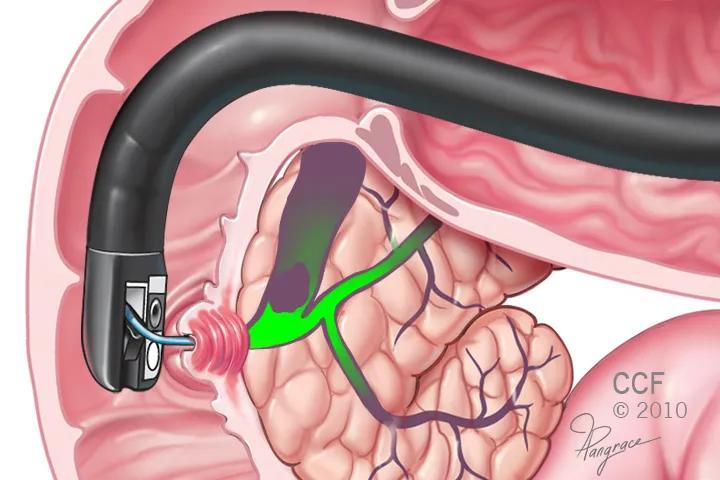
A better way appears to be EDGE — endoscopic ultrasound-guided transgastric endoscopic retrograde cholangiopancreatography (ERCP) — a 40-minute outpatient procedure being performed by advanced endoscopist Prabhleen Chahal, MD.
EDGE utilizes a special endoscope containing both a small camera and an ultrasound probe, which allows the endoscopist to visually distinguish the excluded stomach from the gastric pouch or roux limb. A fistula is made and a stent inserted to recreate the normal anatomy and allow easy access to perform the needed procedure on the pancreas or bile ducts. The stent can be left in place if a patient requires multiple procedures.
Read more about EDGE.
Treatment of gastroesophageal reflux disease (GERD) has typically required medical therapy or laparoscopic fundoplication, both of which are associated with potential safety concerns.
A less-invasive option, transoral incisionless fundoplication (TIF), is being offered at Cleveland Clinic by John Rodriguez, MD, Director of Surgical Endoscopy, and Madhusudhan Sanaka, MD, Section Head of Advanced Endoscopy.
Advertisement
Appropriate candidates are non-obese GERD patients with small hernias (< 2 cm). One of the major advantages of the technique is that it is associated with minimal postoperative recovery time, making it attractive to patients. TIF is also highly effective, producing results that are comparable to surgical and medical therapies.
Read more about TIF for GERD.
A first-ever endoscopic approach for opening fistulas has been developed at Cleveland Clinic and was recently shown to be highly successful in patients with inflammatory bowel disease (IBD). Fistulas can occur in patients with Crohn’s disease and ulcerative colitis, and after restorative proctocoletomy with ileal pouch-anal anastomosis (IPAA). Untreated single-tract fistulas in patients with IBD can develop into complex fistulas, or lead to abscess or pouch failure.
Endoscopic fistulotomy using a needle-knife allows surgeons to go deeper into the bowel than was previously possible with surgical fistulotomy, according to Bo Shen, MD, Medical and Endoscopic Management Director of the Inflammatory Bowel Disease Program at Cleveland Clinic, and his colleague Gursimran Kochhar, MD.
In a series of 29 patients with IBD, the team achieved a 90 percent success rate with endoscopic fistulotomy. Twenty-six patients had complete resolution of fistulas, and only three required surgical intervention after endoscopy. The outpatient procedure takes approximately 20 minutes to perform and is safe when performed in appropriately selected patients — i.e., those with a simple fistula < 3 cm in length.
Advertisement
Dr. Shen and his team are currently drafting guidelines for endoscopic treatment of IBD.
Read more about endoscopic fistulotomy.
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications