Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e7f7c481-2312-4636-bd1f-52cd3c266b94/Machine-Perfusion-Dynamic-Preservation_CCF)
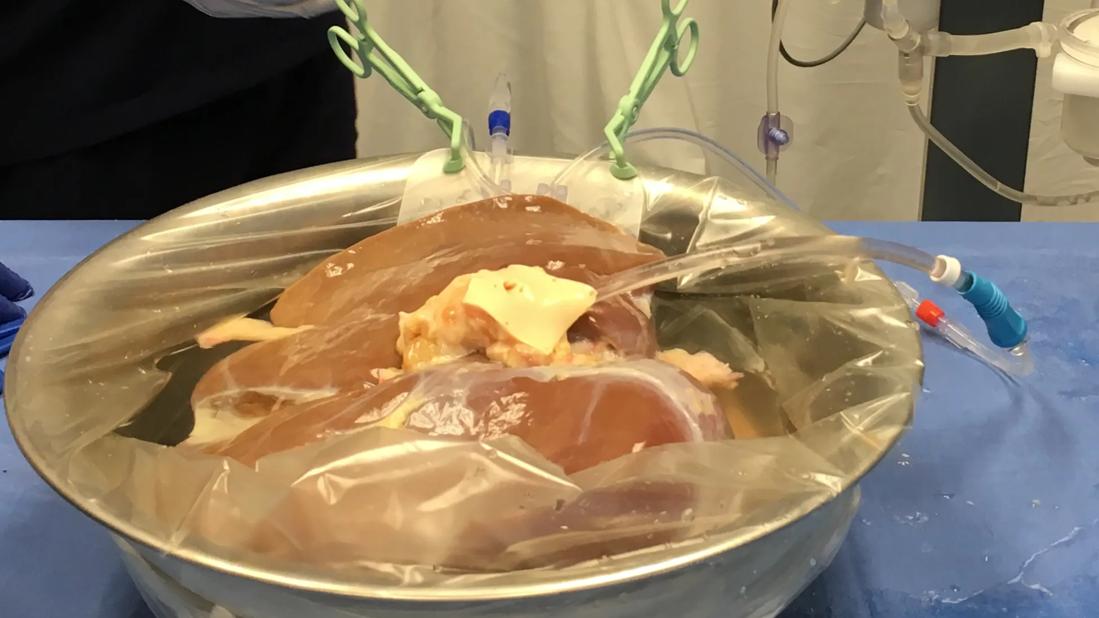
machine perfusion organ image
Approximately three out of four deceased donor liver transplants performed at Cleveland Clinic Weston Hospital now involve the use of machine perfusion, an advanced organ preservation technique that circulates oxygenated blood or other fluids through the donor organ before transplantation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The adoption of machine perfusion methods for dynamic preservation of donor organs is the most exciting development in the field of transplantation in over a decade,” says David J. Reich, MD, Surgical Director of the Liver Transplant Program and Chief of the Innovative Technology and Therapeutics Program for Cleveland Clinic in Florida. “These technologies are allowing for more transplants with better functioning organs while reducing wait times and improving outcomes.”
The Transplant Center at Weston Hospital has experience with both normothermic and hypothermic oxygenated machine perfusion preservation for liver transplantation. Normothermic perfusion (NMP) maintains the organ at body temperature (around 37°C), allowing continuous metabolic activity within the organ prior to transplantation. Hypothermic perfusion involves cooling the organ to a lower temperature, usually below 12°C. This slows down cellular processes and reduces metabolic demand during re-oxygenation.
“Both techniques provide us the opportunity to test, treat and repair donated organs,” says Dr. Reich. “Studies have demonstrated that machine perfusion can outperform static cold ‘icebox’ storage, the traditional preservation method, and results in safer outcomes and increased access to transplant.”
As the national lead investigator for the Bridge to HOPE clinical trial, Dr. Reich delivered an oral late-breaker presentation and two other oral presentations in June at the American Transplant Congress (ATC), the joint annual meeting of the American Society of Transplant Surgeons and the American Society of Transplantation. The ATC presentations also were published in the American Journal of Transplantation.
Advertisement
He reported the findings from the U.S. multicenter randomized controlled clinical trial on the safety and effectiveness of static cold storage (SCS) compared to cold storage followed by hypothermic oxygenated perfusion (HOPE) with the VitaSmart™ system prior to the transplantation of expanded risk criteria donor livers. This trial included both donation after brain death (DBD) and donation after circulatory death (DCD) organs.
Unlike standard criteria donor organs, which come from donors under 50 years old, without certain comorbidities, and who suffer brain death, expanded risk organs are retrieved after circulatory death or come from donors who are older or have certain comorbidities. Such organs are prone to injury during static cold storage.
“Donor livers retrieved after circulatory death experience prolonged hypotension, anaerobic metabolism, and then complete lack of oxygen. The damage makes the recipients particularly vulnerable to ischemia reperfusion injury,” explains Dr. Reich. “This results in higher rates of poor graft function and biliary complications, demonstrating the need for better preservation techniques like HOPE.”
In the Bridge to HOPE trial, Dr. Reich and his research colleagues observed a lower rate of early allograft dysfunction in the HOPE arm (20%) compared to the SCS arm (37%), revealing statistically significant primary endpoint superiority with HOPE. The HOPE group also experienced a statistically significant shorter median hospital stay than the SCS group (8 vs 11 days).
Advertisement
At the time of the ATC presentation, which was just shy of the one-year follow-up period for all subjects, the HOPE arm also demonstrated fewer serious adverse events. This included lower rates of Clavien-Dindo grade >3 events (51% vs 60%) and a reduced incidence of clinically significant DCD ischemic cholangiopathy (11% vs 19%).
“Our safety results are phenomenal, and we are really gratified to see greater organ survival in the DCD liver recipients,” notes Dr. Reich. “The graft failure rate among these recipients was just 7% in the HOPE arm compared to 19% in the SCS arm.”
Since June 2022, the Weston Hospital transplant team has performed more than 65 deceased donor liver transplants benefiting from machine perfusion. “Our Machine Perfusion Program has fueled the doubling of our annual liver transplant volume,” reports Dr. Reich.
Weston Hospital was one of the largest enrollment sites for the Bridge to HOPE trial, completing eight transplants using hypothermic oxygenated perfusion and another seven cases in the cold storage arm.
But the majority of machine perfusion-supported liver transplants at Weston Hospital — about 40 cases — involved the OrganOx metra® device, an FDA-approved NMP system. Researchers at Weston Hospital joined with their Cleveland Clinic counterparts in Ohio to conduct a retrospective cohort study looking at the impact of NMP and acuity circles on waitlist time, mortality and cost in liver transplant. Their findings were published earlier this year in Liver Transplantation.
Advertisement
“Machine perfusion dramatically shortened the median waiting time from listing to transplant and significantly reduced waitlist mortality,” says Dr. Reich.
In another 16 liver transplant cases, patients at Weston Hospital received donor organs preserved and transported using the TransMedics Organ Care System, a normothermic preservation and assessment technology FDA-approved for lung, heart and liver transplantation. “This device may be used during flight, which increases our capacity to bring livers from afar,” explains Dr. Reich.
Most recently, the Weston Hospital team has performed three liver transplants involving donor organs retrieved following normothermic regional perfusion. This method uses extracorporeal membrane oxygenation (ECMO) technology to restore abdominal or abdominal/thoracic circulation within an organ donor who has experienced circulatory death.
“Normothermic regional perfusion is a cutting-edge approach that further allows us to safely increase transplants of DCD organs,” states Dr. Reich.
“As an enterprise, Cleveland Clinic is helping lead the way in organ preservation and rejuvenation,” says Dr. Reich. “Weston Hospital has one of the most advanced Machine Perfusion programs in the region in terms of breadth of techniques and research. With vision from Antonio Pinna, MD, and Charles Miller, MD, our Transplant Center and Enterprise directors, respectively, we’ve invested significant resources into this initiative with the goal of improving access to transplant and outcomes thereafter.”
Advertisement
The Transplant Center at Weston Hospital now has a designated machine perfusion room across from a specially equipped transplantation operating room. Paralleling growth of the new perfusion program and increased transplant volumes, the hospital opened a 28-bed inpatient unit on the 5th floor of the hospital’s Tower Building for the co-location of patients receiving pre- and post-transplant care.
“Our transplant team includes five full-time inpatient transplant nurse practitioners, who have an office in the center of the unit on the 5th floor,” describes Dr. Reich. “They are highly attuned to the special needs of our patients, and their proximity makes providing care especially efficient and effective.”
In addition to dedicated clinical resources, Weston Hospital has a new machine perfusion research lab on campus and a full-time clinical research fellow.
“Together with our Ohio colleagues, we are exploring new methods of organ viability testing, which will allow us to better guide donor organ selection and recipient matching,” Dr. Reich adds. “In the not-too-distant future, we plan to establish an organ donor care center and organ therapeutics and reconditioning facility, as part of our innovative and comprehensive efforts to increase transplantations and improve outcomes for patients.”
Advertisement
Nonthermal technique reduces bleeding and perforation risk
Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer
PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital
Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence
Noninvasive modality gains ground in United States for patients with early-to-moderate disease
Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases
Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules
Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.