Three years ago neurosurgeon Hamid Borghei-Razavi, MD, joined Cleveland Clinic Weston Hospital with the intent to establish the Minimally Invasive Cranial and Pituitary Surgery Program, mirroring a similar program launched in 2014 at Cleveland Clinic in Ohio. As director of the program, which is part of Cleveland Clinic Florida’s Brain Tumor Center in Weston, he leads a multidisciplinary team that provides minimally invasive treatment options for pituitary and other skull base pathologies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We’ve come far in a very short time,” says Dr. Borghei-Razavi, noting the Florida program’s patient volume has more than tripled since 2019. “We are conducting more extensive endoscopic tumor removals than ever before, including tumors invading the cavernous sinus and those with vascular involvement.”
Next February Dr. Borghei-Razavi will share lessons learned by the Cleveland Clinic Florida team when he presents at the North American Skull Base Society (NASBS) 32nd Annual Meeting in Tampa, Florida. His presentation on establishing an endoscopic skull base surgery program will cover the necessary building blocks, including the value of mentors, leadership support, the role of a multidisciplinary approach, and essential infrastructure.
Dr. Borghei-Razavi credits the Florida program’s rapid success to its integration with the Ohio program. The two teams conduct joint pituitary tumor board meetings each month, co-host education days, and participate in other opportunities to share best practices. “Our goal is to provide patients the same quality of care regardless of location,” says Dr. Borghei-Razavi, who completed his fellowships in neurosurgical oncology and advanced open and endoscopic skull base surgery at the Cleveland Clinic Neurological Institute in Ohio before moving to Florida.
He also cites as an invaluable resource the local leadership and support of Badih Adada, MD, Chair of the Cleveland Clinic Florida Neurological Institute and a well-known expert in skull base, epilepsy and vascular neurosurgery, as well as the guidance of his mentors, Pablo Recinos, MD, Section Head of Minimally Invasive Skull Base Neurosurgery in Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center, and Varun Kshettry, MD, Director for the Advanced Endoscopic & Microscopic Neurosurgery Laboratory in Ohio.
Advertisement
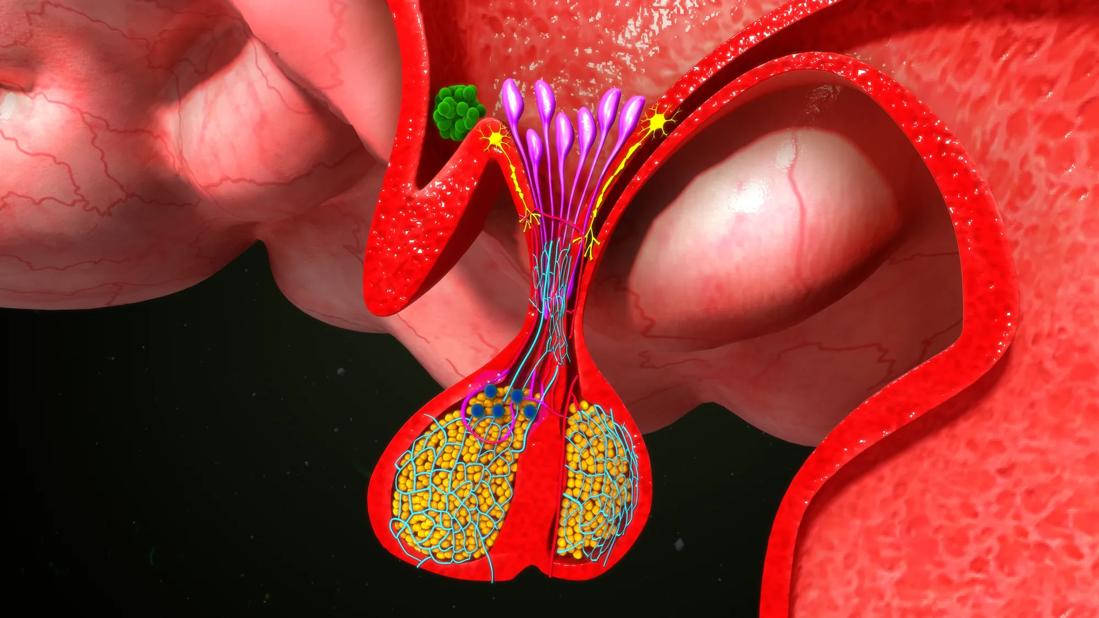
The Florida program brings together five medical specialties to diagnosis and treat patients with functioning and nonfunctioning pituitary adenomas, craniopharyngiomas, meningiomas, skull base defects, and cancers. Depending on the type and location of the lesion, the care team may include a neurosurgeon, a rhinologist, an endocrinologist, radiation oncologist, and a neuro-interventional radiologist.
“Like a basketball team moving the ball down the court, we all have an important role to play in the care of the patient,” says Dr. Borghei-Razavi. “In particular, our two-surgeon approach, where a neurosurgeon and ENT operate together, allows us to endoscopically treat very complex cranial conditions and achieve better outcomes.”
Today most pituitary surgeries at Cleveland Clinic Weston Hospital are performed endoscopically. “Very few require a microscopic or combination approach, such as some giant pituitary adenomas with extreme lateral extensions,” says Dr. Borghei-Razavi.
Other skull-base tumors also may be endoscopically resected, including chordoma, chondrosarcoma, and intraventricular tumors and cysts. If surgery is not appropriate, such as for certain recurrent tumors or those attached to blood vessels, the team’s radiation oncologist may recommend stereotactic radiosurgery.
In addition to using new generation endoscopes, the Cleveland Clinic Florida team employs advanced navigation techniques and intraoperative fluorescein to improve visualization of the surgical field. “With fluorescence-guided surgery, we are able to better visualize the vasculatures and avoid manipulation and injury of the carotid artery and other sensitive structures during tumor resection,” explains Dr. Borghei-Razavi.
Advertisement
Earlier this year, he and his Florida colleagues also incorporated the use of augmented reality (AR) technology to plan tumor surgeries. The navigation system combines surgical planning software and MRI data to create 3D anatomical models and 2D image slices. An AR head-mounted display allows the surgical team to collaborate in real time as they evaluate approaches and plan the best surgery route based on the patient’s unique anatomy.
“We’ve been using this spatial computing technology since the spring, and I’m convinced it has made surgical planning easier and surgery safer,” says Dr. Borghei-Razavi. His team is the first in the Cleveland Clinic enterprise to use this new tool.
According to Dr. Borghei-Razavi, the Florida team also began tracking patient-reported clinical outcomes this summer for patients undergoing cranial surgery. These outcomes focus on the impact of disease on a patient’s quality of life and how care affects functions and limitations associated with a disease.
“The data we capture will allow us to systematically look at the impact our care has on the lives of patients, identify factors that influence outcomes, and help define best practices that can improve care in the future,” he says.
While outcomes tracking has the potential to advance care in the long-term, the Cleveland Clinic teams in Florida, Ohio and Abu Dhabi are working together to share current best practices and treatment innovations. In December they are hosting a Cleveland Clinic Microscopic and Endoscopic Skull Base Surgery Workshop for neurosurgeons and otolaryngologists at the Cleveland Clinic Florida – Pauline Braathen Neurological Center located on the Weston campus. Attendees will receive hands on experience in different complex approaches and contemporary management issues in patients with skull base pathologies.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.