Advertisement
Consider post-exercise ABI in all patients with claudication
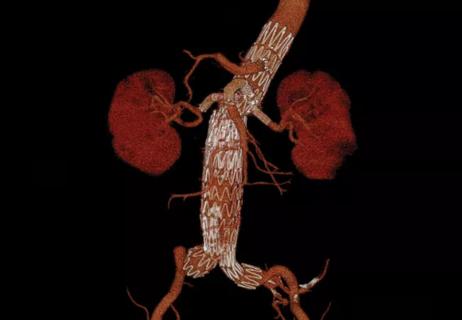
Could post-exercise measurement of the ankle-brachial index (ABI) be more predictive of lower extremity revascularization rates in peripheral artery disease (PAD) than the typically performed resting ABI measurement? A disconnect between results with resting ABI when testing for PAD and when grading PAD severity led a Cleveland Clinic research team to take a closer look. Their findings were recently published in JACC: Cardiovascular Interventions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
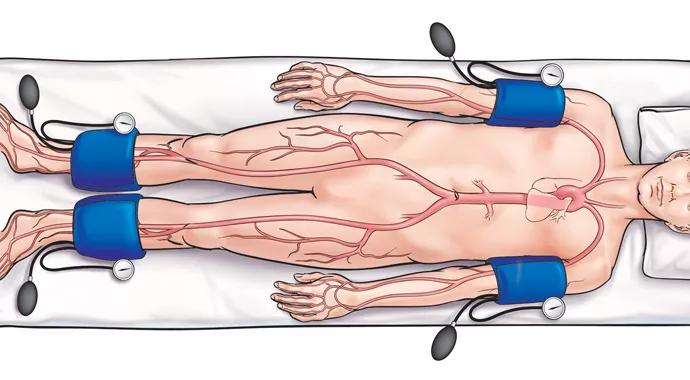
Resting ankle-brachial index (ABI) is the most common test for diagnosing and grading the severity of lower-extremity atherosclerosis, and an important tool when considering revascularization in PAD patients. Current American College of Cardiology/American Heart Association (ACC/AHA) guidelines do not recommend post-exercise ABI measurement when resting ABI is abnormal.
But Mehdi Shishehbor, DO, MPH, PhD, Director of Endovascular Services in Cleveland Clinic’s Robert and Suzanne Tomsich Department of Cardiovascular Medicine, says post-exercise ABI may more accurately represent blood flow when patients are experiencing claudication — typically pain, tightness or discomfort that occurs in the calf muscles when walking but resolves with resting.
“When patients come in complaining of pain in the calf, the test typically performed in most U.S. centers is a resting ABI,” says Dr. Shishehbor, principal author of the new study. “There is a disconnect because the patient is complaining of symptoms when they walk, but the test for blood flow is performed only at rest. Our hypothesis was that to better understand blood flow and its relation to a patient’s symptoms, we should add an exercise test to reflect that.”
To test that hypothesis, Dr. Shishehbor and colleagues conducted a retrospective analysis of 2,791 consecutive patients who underwent both resting and post-exercise ABI testing at Cleveland Clinic over a five-year period. Their key findings included the following:
In addition, patients who presented with both abnormal resting and abnormal post-exercise ABI had a trend toward higher mortality rates, as well as significant increases in major adverse cardiovascular outcomes.
Ideally, Dr. Shishehbor says, patients should undergo resting ABI, then walk on a treadmill for five minutes at a 12.5 percent grade at 2 miles per hour or until symptoms force them to stop, and then undergo a post-exercise ABI measurement. The combined tests provide a truer sense of blood flow in the legs.
As the ABI is the ratio of systolic blood pressure measured at the ankle to that measured at the brachial artery in the arm, it can be expressed as a percentage value that can exceed 100, with ranges typically judged as follows:
Advertisement
When resting ABI is used alone, most patients present in the mild to moderate categories. For example, a patient might present at 70 percent with resting ABI, but his or her post-exercise ABI might be only 20 percent.
“The physician may act differently if they see 20 percent rather than 70 percent,” Dr. Shishehbor notes. “That 70 percent does not reflect blood flow when the patient has symptoms. It doesn’t make sense to rely solely on a test we perform when the patient doesn’t have symptoms.”
But there are challenges to convincing centers to add post-exercise ABI as a standard of care.
Some centers, Dr. Shishehbor says, have patients perform a repetitive active pedal plantar flexion technique, which has results very comparable to those of the ideal method of having patients walk on a treadmill for five minutes at a 12.5 percent grade at 2 miles per hour. Unfortunately, time and insurance constraints prevent many centers from offering the treadmill exercise ABI.
Advertisement
Another challenge are the current ACC/AHA guidelines, which recommend post-exercise ABI only when resting ABI is normal and there is a high suspicion that a patient has PAD.
“We are suggesting every patient with claudication should be considered for post-exercise ABI,” Dr. Shishehbor says. “It’s a very safe procedure and there is not a lot of expense associated with doing it.”
Dr. Shishehbor points out that his team’s new analysis is only the second study to look at the clinical effect of abnormal post-exercise ABI on lower extremity revascularization, and one of only a handful of studies to investigate the prognostic implications of abnormal post-exercise ABI.
He is now searching for funding to take his research to the next level — a randomized study assigning patients with claudication symptoms to measurement of either resting ABI alone or resting ABI plus post-exercise ABI. He says that type of prospective study would help definitively determine outcomes according to the tests used, how they affect the types of intervention and treatment, and whether there are resulting differences in quality of life and health outcomes.
Advertisement
Advertisement

Further acute testing not needed if ECG and high-sensitivity troponin are negative

Scott Cameron, MD, PhD, also brings wide-ranging research interests to bear

Pioneering U.K. vascular surgeon joins Cleveland Clinic

AHA statement is first comprehensive document on perioperative stroke reduction
Recognition reflects prioritization of long-term patient outcomes

Recommendations help distinguish exercise-induced remodeling from pathology

JACC review highlights factors unique to women, ways to tailor management
Pushing the envelope in ablation of atrial fibrillation, ventricular tachycardia