Communication is particularly critical in this often-misdiagnosed disorder

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/88de17eb-ccb9-4d69-99bf-a505751610a1/NEU_2865231_06-02-22_030_LDJ)
EEG monitoring
By Becky Bikat S. Tilahun, PhD, and Jocelyn F. Bautista, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This is part 1 of a two-part article reprinted (without references) from the Cleveland Clinic Journal of Medicine (2022;89[5]:252-259). Part 2 addresses treatment of psychogenic nonepileptic seizure. The open-access and fully referenced original article is available at ccjm.org/content/89/5/252.
A 19-year-old right-handed man who had meningitis at age 12 presented with seizures that had begun 12 months earlier. He described the seizures as bilateral arm-stiffening and stuttering speech, followed by rocking movements of the head and trunk that waxed and waned over 30 to 40 minutes. He said he never lost consciousness. He identified lack of sleep and stress as triggers.
The patient was brought to a local emergency department in the midst of a prolonged seizure and was treated with intravenous lorazepam. He was evaluated by a local neurologist, who prescribed levetiracetam for the seizures. Results of routine outpatient EEG and brain MRI were normal. He continued to have seizures, despite escalation of levetiracetam doses.
He was admitted to the epilepsy monitoring unit for continuous video EEG monitoring. Several typical episodes were recorded and confirmed by family members and the patient. The episodes were characterized by gradual onset of irregular jerking of his head and arms, followed by arm and truncal stiffening and initial eyes-closed unresponsiveness. He then gradually started following commands but continued to have irregular bilateral jerking movements for 10 more minutes. No epileptiform EEG changes were seen before, during or after the episodes. Likewise, interictal EEG over 72 hours was normal. He was diagnosed with psychogenic nonepileptic seizure (PNES).
Advertisement
Previously known as pseudoseizure, PNES resembles epileptic seizures in symptoms and signs but is not caused by abnormal epileptiform electrical activity in the brain. Instead, this disorder is a manifestation of underlying psychological distress and unresolved emotions. Many people diagnosed with PNES meet the criteria for conversion disorder (also known as functional neurological symptom disorder) or other somatoform disorder, and others meet the criteria for dissociative disorder.
Multiple terms have been used to describe PNES, including dissociative seizure, functional seizure, stress seizure and nonepileptic attack, reflecting the difficulty of finding a term that respectfully indicates both the psychological nature of the condition and its superficial similarity to epilepsy. The long-entrenched term pseudoseizure has been misinterpreted by patients and physicians as meaning the patient is “faking” or feigning the seizures. Unfortunately, this view has negatively influenced how some healthcare providers treat patients with PNES.
Importantly, there are other causes of nonepileptic events besides PNES — e.g., syncope, migraine (which can be accompanied by transient focal neurologic symptoms and signs), paroxysmal dystonias and other movement disorders. Rarely, a nonepileptic event is due to intentional deception as in factitious disorder or malingering. In some people with developmental or intellectual disabilities, nonepileptic events are behavioral or attention-seeking. PNES is distinctly different in that it is not conscious or intentional.
Advertisement
The pathophysiology of PNES is unclear, but the literature suggests that PNES is a network disorder affecting sensorimotor processing, emotional regulation and neural responses to stress. Functional neuroimaging studies provide some evidence that people with PNES have abnormalities in limbic brain structures including the amygdala, hippocampus, parahippocampal gyrus, insula, cingulate cortex and prefrontal cortex.
PNES can develop at any age but is most common between ages 15 and 35. The disorder is more common in women, and particularly in women who have been victims of abuse. Childhood abuse (sexual, emotional or physical) is strongly correlated with subsequent development of PNES. Psychiatric disorders such as depression, anxiety and posttraumatic stress disorder are also commonly seen in patients with PNES.
Early studies estimated the prevalence of PNES at 2 to 33 per 100,000. A 2021 systematic review calculated the incidence of PNES in the United States at 3.1 per 100,000 per year, and the prevalence at 108.5 per 100,000. In comparison, epilepsy has an incidence of 62 per 100,000 per year and a prevalence of 1.2%, or 1,200 per 100,000.
From 25% to 35% of patients referred to epilepsy monitoring units for video EEG are diagnosed with PNES. The disorder is often misdiagnosed as epilepsy, placing patients at risk of iatrogenic complications related to unnecessary antiseizure medications and inappropriate medical interventions such as intensive care unit admission, benzodiazepine administration and oral intubation.
Advertisement
PNES is associated with poor quality of life and high rates of unemployment and disability. Mortality rates are also higher in people with PNES than in the general population, with one study finding that 20% of deaths in those with PNES under age 50 were due to suicide.
A comprehensive history and video EEG during a typical seizure are the gold standard for diagnosing PNES. There should be no epileptiform abnormalities on the EEG before, during or after a typical event.
Absence of EEG changes alone, however, is not always diagnostic. EEG must be interpreted in the context of clinical signs and symptoms. Features of seizure semiology or symptomatology that are highly predictive of PNES include the following:
Fluctuating patterns of movement are also suggestive of PNES, as are distractibility, crying or stuttering during the seizure.
No one sign is 100% specific for PNES. For instance, out-of-phase limb movements and pelvic thrusting can occur in frontal lobe epileptic seizures, without a clear ictal EEG change.
Video EEG is most helpful when there are motor signs or decreased responsiveness, but like most diagnostic tools, video EEG has limitations. For instance, if the onset of the seizure is not captured on video, postictal behavior can be confused with PNES.
Importantly, video EEG is less useful when the patient has only subjective symptoms, because epileptic aura (with purely subjective symptoms) can be scalp EEG-negative. In addition, certain epileptic seizures can be scalp EEG-negative due to movement artifact or because scalp EEG has difficulty recording from deeper areas of the brain. In these cases, referral to a comprehensive epilepsy center is recommended. As mentioned earlier, other nonepileptic events to consider are migraine, vertigo, syncope, movement disorder (e.g., paroxysmal dystonia and dyskinesia) and sleep disorders such as narcolepsy, cataplexy and parasomnias.
Advertisement
About 10% of patients with PNES also have epileptic seizures, so when the patient or the patient’s family describes more than one seizure type, it is crucial to record examples of all seizure types. Once it is confirmed that a patient has both PNES and epileptic seizures, showing the patient and family videos of the seizure types captured with video EEG, and highlighting key features of both seizure types, will help them distinguish PNES from epileptic seizures once they leave the monitoring unit.
Presenting the diagnosis to the patient is typically the job of the neurologist who has interpreted the video EEG. Communicating the diagnosis effectively is crucial and can be therapeutic in the short term. However, if learning the diagnosis leaves the patient angry or confused, PNES and other psychiatric symptoms will likely worsen.
A survey of primary care and emergency medicine physicians found that 38% believed that episodes of PNES are intentionally produced or faked, and 63% did not feel video EEG was needed to confirm a diagnosis of PNES. The misperception that PNES is intentionally feigned is likely to result in mismanagement of the condition.
Many patients with PNES say the diagnosis is confusing and distressing, and they feel misunderstood, mistreated and blamed when they seek medical care. About a quarter feel the diagnosing doctor does not understand their PNES symptoms. Receiving a diagnosis of PNES can be particularly confusing for patients who were previously diagnosed with epilepsy and treated for years with antiseizure medications. When their diagnosis is changed from epilepsy to PNES, patients find the news distressing because they perceive the burden of recovery is shifted from the doctor’s shoulders to theirs. Misperceptions about PNES and poor physician-patient communication certainly add to the emotional struggles of patients and can lead to resistance to mental health recommendations.
Since many people with PNES have a history of trauma and abuse, perceived or actual mistreatment by medical providers (via poor communication of the diagnosis) can traumatize them yet again and makes it more likely they will reject the diagnosis. Various communication strategies have been proposed, but the most important component is to deliver the diagnosis with empathy and clarity.
Key points in discussing the diagnosis with the patient are to acknowledge that their symptoms are real and can be frightening and disabling. It can be reassuring to know that they are not alone and that PNES is a diagnosis that is common in epilepsy monitoring units.
The discussion should also clarify that the patient does not have epilepsy and does not need antiseizure medications (assuming the patient does not have comorbid epileptic seizures). Rapid titration off antiseizure medications at the time of diagnosis is associated with better outcome than with delayed titration.
It is helpful to discuss the role of emotions and stress in producing physical symptoms, similar to the way anxiety can cause abdominal pain or headaches. Finally, it is essential to let the patient know that with treatment PNES can resolve, and that seizure control with a return to normal function should be the goal. These steps are summarized in Figure 1.
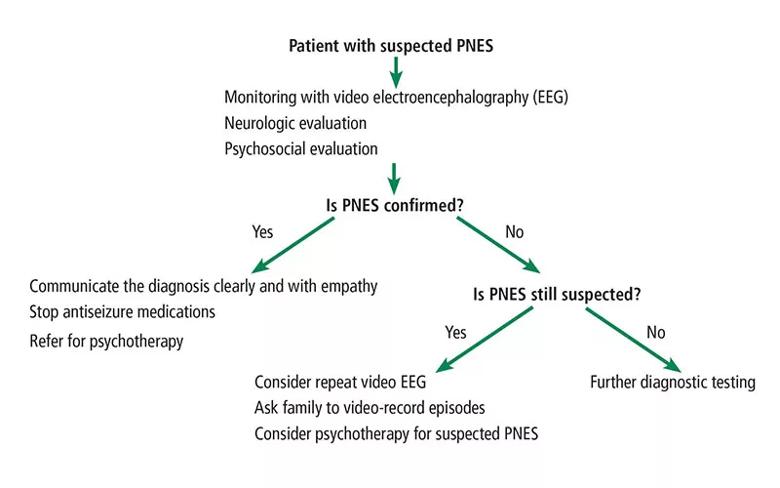
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1aaf9e2c-8f5a-41b2-81c6-7918b3a5b4d7/22-NEU-3140064-CQD-Inset1-800x500-1_jpg)
Figure 1. Algorithm for diagnosing psychogenic nonepileptic seizure (PNES).
Returning to our case patient, we talked to him further and found that he began to have depressive symptoms after his grandmother died, four years before the onset of his seizures. In the year after her death, he began to drink alcohol and abuse drugs.
After graduating from high school in May 2020, he joined the military, but soon after, he tested positive for COVID-19 and was placed in quarantine. Being diagnosed with COVID-19 early in the pandemic when there was so little information available was a traumatic experience for him. He felt helpless and had severe crying spells because he thought he was going to die. His quarantine “buddies” were likewise experiencing depressive symptoms, and he witnessed multiple episodes of self-injurious behavior among the other recruits. While in quarantine, he developed seizures and was hospitalized.
He was eventually discharged from the military and returned home. He then enrolled in college, where he struggled with his classes and had a series of failed romantic relationships.
In the epilepsy monitoring unit, he was diagnosed with anxiety in addition to PNES. The diagnosis of PNES was explained in the context of his recent stressors, and though he was tearful, he said he felt relieved to know he did not have epilepsy. He and his family understood and accepted the PNES diagnosis, and outpatient psychotherapy was scheduled.
Dr. Tilahun is a clinical psychologist with Cleveland Clinic’s Center for Behavioral Health and Epilepsy Center. Dr. Bautista is a neurologist in Cleveland Clinic’s Epilepsy Center.
Advertisement
New study highlights the need for plain-language prompting and human oversight in addiction care communication
What hospital clinicians get right — and wrong — when diagnosing depression and delirium
Swift, aggressive thiamin therapy may be key to preventing long-term neurological injury
Case underscores potential dangers of combining psychedelics with tranylcypromine and stimulant medications
Researchers explore how changes in the gut microbiome influence the brain's reward response to alcohol
Researchers explore new avenues for the management of psychiatric illness in patients with seizure disorders
Addiction experts use decades of research and clinical experience to help patients overcome substance use disorders
Specialized course helps APPs navigate clinical concerns and interpersonal skills