Complex, bidirectional interactions exist between cancer, therapy, toxicities and eating behaviors

The toxicities that commonly result from chemotherapy and radiation often have a negative impact on eating. This in turn reduces patients’ food intake during a time when they particularly need adequate nutrients to foster energy and healing.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Investigating this complex relationship between cancer treatment’s toxicities and reduced nutritional intake has been a passion for Peter Anderson, MD, a pediatric oncologist at Cleveland Clinic Children’s, since he was the pediatric bone marrow transplant attending physician at the University of Minnesota in 1991. “Eleven of the 12 children and adolescents were on morphine drips for painful mucositis,” Dr. Anderson recalls. “I felt terrible that these kids had to go through such pain to get a lifesaving procedure.”
The situation inspired Dr. Anderson to research what might help mucosal healing. He found the answer in the field of surgery regarding wound healing — good nutrition. “The secret ingredient in the nutrition was glutamine, which is an amino acid in proteins. It’s not in the TPN that we give during bone marrow transplant,” he says.
Because glutamine isn’t particularly soluble or good tasting, Dr. Anderson compounded it in a sugar suspension and found his creation helped foster mucosal healing during chemotherapy. Three patents and multiple successful trials later (including three randomized, double-blind, placebo-controlled trials), he and several colleagues turned his glutamine disaccharide discovery into a commercially available powder for cancer patients called Healios.
The opportunity to summarize and share his decades of experience in an open source journal was one Dr. Anderson couldn’t pass up. With the assistance of seven other researchers, including Stefanie Thomas, MD, he headed up a review published in Nutrients discussing strategies to mitigate cancer therapy toxicities and improve eating behaviors.
Advertisement
“Basically, it gives our philosophy, which is instead of running the same play and getting the same toxicity with each cycle of chemotherapy, it helps to ask the embarrassing, hard question: What can we do better?” Dr. Anderson says. “It’s not just giving chemo and radiation reliably with the same dose and schedule. It’s understanding the effect on normal tissues and how to promote healing and finding the opportunities to do that.”
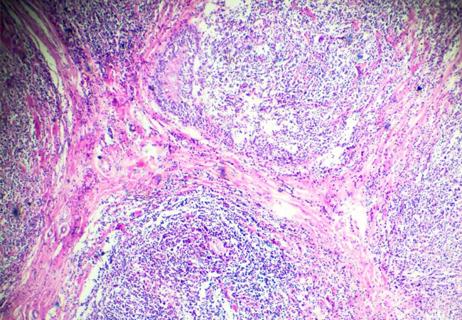
In Figure 1 of the review, the bidirectional and complex nature of cancer therapies (surgery, chemotherapy and radiation), toxicities and eating behaviors is pictured. This figure was created thanks to “one of our astute reviewer’s comments. She said, ‘It’s not that cancer affects the therapy; sometimes the therapy affects the cancer, and the same with the toxicities,’” says Dr. Anderson. “If you have such bad mucositis that you can’t swallow, it affects your eating behavior, and once you don’t have enough nutrients, then you’ve set yourself up for more toxicity. That’s why it’s so complicated.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/efb17d5e-a9c3-41e8-afbd-5b926ff164a5/Anderson-Fg-1_jpg)
Dr. Anderson also discusses “vicious and virtuous cycles.” A vicious cycle is repeating the same treatment over and over again and getting the same toxicity every time. Conversely, a virtuous cycle involves slowing down to find answers to make therapy less toxic for the next cycle.
“You review symptom control and weight trends just before the cycle,” Dr. Anderson says. “Do you need better antiemetics? Do you need a dietitian to talk to the patient? How should they communicate their concerns? And then you put it into practice. You adjust before each cycle so you’re not reacting, you’re proactive.”
Advertisement
Strategies to improve eating behaviors in patients receiving chemotherapy and/or radiation are detailed in the review. These include:
“The worst-case scenario is bone marrow transplant, where you give the highest doses and get the most toxicity,” says Dr. Anderson. These patients especially need to eat constantly and stay active in order to heal. “The best transplants I’ve seen are people who have maintained their nutrition and strength, something that the patient can certainly do,” he says.
One approach Dr. Anderson uses is to tell patients right away at diagnosis that weight loss can be problematic. He explains that he’ll start getting worried if they lose 5% of their body weight. And if they lose 10%, he tells them they’ll need either an NG tube or a G-tube. In practice, if a patient loses 5%, he has them meet with a nutritionist for a G-tube “show and tell.”
“I’ve seen when people lose 10%, they’re really having a lot more toxicity than they need. Then we’ll put in the G-tube and within a few weeks, they have less fatigue and feel much better, so I put that line in the sand — don’t lose more than 10% or we’ll have that discussion,” Dr. Anderson says.
Dr. Anderson has additional advice to encourage eating, such as:
Advertisement
The review summarizes chemotherapy regimen variables to kill cancer cells with better normal tissue tolerance (Table 1). It also outlines radiation damage associations with variables and considerations regarding damage to tumors versus less side effects on normal tissue (Table 2).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a7cf7df4-2e9d-4281-b32e-018508cc6aa3/Anderson-Tbl-1_jpg)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a900526d-2bc2-4234-8186-929310ff5773/Anderson_Tbl_21_jpg)
Nausea and/or vomiting are common side effects of chemotherapy. The review lists causes of nausea and vomiting along with reduction agents and mitigation strategies, considerations and references (Table 3).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8f379417-5343-4c4b-9672-1bc8cffc54c6/Anderson_Tbl_31_jpg)
Dr. Anderson says the current guidelines aren’t adequate for care. “The reality is oncologists are so busy, all we can do is write the orders for chemotherapy in the schedule and say we’re providing standard of care,” he says. “But toxicity shouldn’t be part of the package deal.”
For example, Dr. Anderson says assigning nutritionists to help patients should be routine. “Another gap in care is trying to be proactive,” he says. “Probably the best thing that I’ve done is to get information between cycles of chemotherapy about what could be improved. There should be some mechanism to do that.” He personally uses a Word document to summarize changes to make for the next cycle and to help him prepare for visits in advance.
Outpatient chemotherapy is an area Dr. Anderson advocates for because outpatient treatment results in less toxicity, better eating and more rest for the patient than being in the hospital. He gives this example: Alexa Plutt, PharmD, then a pharmacy resident at Cleveland Clinic in pediatrics, noticed after this review was published that there was a difference in toxicities between inpatients and outpatients who were getting the same chemotherapy.
Advertisement
Plutt then created a retrospective review of 10 pediatric patients receiving either continuous infusion (outpatient) or inpatient bolus administration of ifosfamide/mesna at Cleveland Clinic Children’s. “She looked at factors like fever, neutropenia and number of red cell and platelet transfusions. If they were outpatient, there was no fever, neutropenia or transfusions, but if they were inpatient, it was quite common,” says Dr. Anderson.
Because it is a safe “food” reduces toxicity, he would also like to see more caregivers, pharmacies and medical oncologists make Healios available, the glutamine disaccharide powder he developed, available. Dr. Anderson believes more infusion nurses, physician assistants and advanced nurse practitioners are needed to focus on reducing toxicity. “They’ll have more time and inclination to do this than the doctors,” he says. “And if we can empower and educate infusion nurses to do the same thing, they spend a lot of time with the patients and get to know them well, so they could be seen as educators too.” In his pediatric practice, Dr. Anderson has a nurse coordinator who not only makes appointments, but also educates patients throughout their therapy.
According to Dr. Anderson, there are many opportunities for further research in this area. “If there are ways to improve care, delivery or consistency of care, we should find them,” he says.
Editor’s note: All tables and figures featured in this article were republished under the Creative Commons Attribution 4.0 International (CC BY 4.0) license. They originally appear in Anderson PM, Thomas SM, Sartoski S, Scott JG, Sobilo K, Bewley S, Salvador LK, Salazar-Abshire M. Strategies to Mitigate Chemotherapy and Radiation Toxicities That Affect Eating. Nutrients. 2021; 13(12):4397.
Advertisement

Key themes and insights into the family-caregiver experience

First-of-its-kind clinic for immune-related adverse events supports oncologists in managing severe side effects

Early communication between oncologists and ophthalmologist warranted

Variables affect nuances of the conversation

Driving advances in cancer care
Challenges emerge with application of interim PET scans

Helping patients with cancer struggling with depression, anxiety and other mental health issues