New tools and protocols to improve care
Written by Rachel Scheraga, MD; Eduardo Mireles-Cabodevila, MD; and Joshua Veith, MD, MSCE
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The pathobiology of acute respiratory distress syndrome (ARDS) is characterized by innate immune infiltration into the alveolar space for clearance of pathogens, dead cells and debris. However, how the innate immune cells sense the injured alveolar extracellular matrix to regulate their function remains an unanswered question.
As a NHLBI/R01-funded investigator, Dr. Rachel Scheraga and her group have been studying the mechanosensitive, cation membrane channel, transient receptor potential vanilloid 4 (TRPV4) and its role in the injured and stiffened lung from ARDS. Her initial work found that TRPV4 in macrophages was required for macrophage phagocytosis and an anti-inflammatory cytokine profile in ARDS lungs (Figure 1). They have since expanded their studies to a clinically relevant Pseudomonas aeruginosa pneumonia model and found that TRPV4 protected the lung from injury.
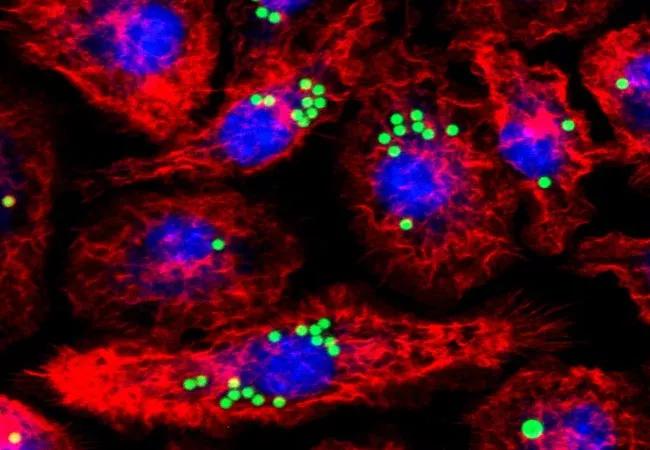
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/693f29ca-2f79-405b-9137-d40d933aa02d/23-PUL-4178617-CQD-DM-Stretching-boundaries-ARDS-Hero-1_jpg)
Figure 1. Macrophages engulfing IgG coated fluorescent latex beads after LPS treatment with immunofluorescent staining for the actin cytoskeleton with Phalloidin. Red-Phalloidin, actin cytoskeleton, green-IgG coated beads, blue-DAPI, nuclei.
This work has subsequently led to them further characterize downstream molecular mechanisms by which TRPV4 in macrophages regulates phagocytosis and cytokine secretion. Future studies from her group are trying to understand the differential TRPV4 gene expression in sub-sets of pulmonary macrophages and the effect of lung injury from sepsis in humans, which may be useful as therapeutic target for lung injury.
Advertisement
The unique biology uncovered by Dr. Scheraga’s laboratory has sparked interest in a number of our clinical investigators to explore how lung stretch and stress at the bedside may be used as a tool to improve delivery of care for ARDS patients.
Work from Robert Chatburn MHHS, RRT-NPS, FAARC, and Eduardo Mireles-Cabodevila MD, FCCM, CHSE has resulted in a better understanding of the intricacies of the application of mechanical ventilation. Their work has generated more than 50 publications and book chapters helping organize the field of mechanical ventilation.
This growth in knowledge and understanding in critical care has led to the formation of the Standardized Education for Ventilatory Assistance (SEVA) course and the Ventilator Interest Research GrOup (VIRGO), an interprofessional and interdisciplinary group at Cleveland Clinic (Figure 2). The focus of VIRGO is to promote research in the field of mechanical ventilation. As part of these efforts, we developed an ARDS protocol that emphasized Low Tidal Volume Ventilation, PEEP optimization and prone position ventilation as the three-cornerstone evidence-based practices (EBPs) of early ARDS care.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/77846495-bb5a-448f-bd0c-43864c850b64/23-PUL-4178617-CQD-DM-Stretching-boundaries-ARDS-Inset-1-1_jpg)
Figure 2. Schematic of VIRGO group that includes the network, standardization, research, education and implementation.
These protocols and their application have motivated Joshua Veith, MD, MSCE to utilize the principals and methods of implementation science to evaluate for unmet barriers of protocolized ARDS care and identify strategies essential for protocol success. He recently received a Healthcare Delivery and Implementation Science Center grant to conduct semi-structured interviews of ICU providers.
Advertisement
Thematic analysis and the CFIR-ERIC Implementation Strategy Matching Tool were used to define the current state and identify gaps and opportunities in implementation strategy selection. An overarching theme emerged demonstrating there is a need for data-informed continuous improvement infrastructure to overcome existing barriers to protocolized ARDS care.
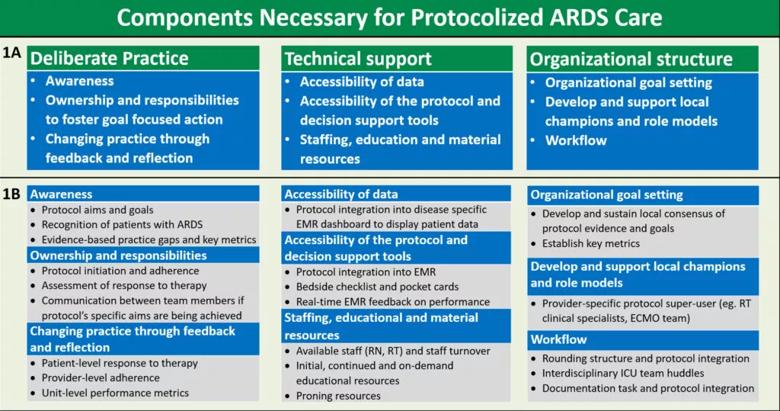
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/eead13ec-0ddd-4561-ae8a-e7db0ccb94d2/23-PUL-4178617-CQD-DM-Stretching-boundaries-ARDS-Inset-2-2-1024x539_jpg)
Figure 3. Themes derived from key barriers and facilitators to use of the ARDS protocol into three main components necessary for successful protocolized ARDS care (1A) with potential targets for future data-informed continuous improvement efforts (1B).
Our study identified three main components necessary for protocolized ARDS care: deliberate practice, technical support and organizational structure. Barriers and facilitators of protocolized ARDS care were categorized within these components as potential targets for future data-informed continuous improvement efforts (Figure 3).
Our team has operationalized our findings and created a Mechanical Ventilation Dashboard capable of providing data-informed continuous improvement. This tool will be used to overcome local barriers utilizing the three-pronged approach of fostering deliberate practice, technical support, and organizational structure. Application of this approach holds promise to improve protocolized care in other complex disease states cared for in the ICU.
Advertisement
Advertisement
Case study illustrates the potential of a dual-subspecialist approach
Endoscopic balloon dilation during pregnancy helps optimize outcomes
Surgery is typically the only option for the most severe cases, but a minimally invasive procedure is reducing morbidity and recovery time for patients
Cleveland Clinic pulmonologists share a framework for how to implement effective clinical protocols to standardize evaluation and management of complex acute respiratory distress syndrome
A public health tragedy with persistent pathophysiological and therapeutic challenges
Recent breakthroughs have brought attention to a previously overlooked condition
Findings show profound muscle loss variance between men and women
For the first time, risk is shown after accounting for underlying contributions of pulmonary disease