Moving from open procedures to minimally invasive surgeries, robotics and lasers

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic has been at the forefront of advances in urogynecology over the past 25 years, most prominently taking the lead in converting open procedures to minimally invasive surgeries. Our team adopted new techniques early on, and has been become well known for studying these techniques in randomized clinical trials. We are also part of the Pelvic Floor Disorders Network, a group of top medical centers in the United States that has received numerous NIH/NICHD grants to perform prospective trials in the management of women’s pelvic floor disorders, which affect at least 10% of women ages 20 to 39 years, increasing with age to at least 50% of women ages > 80 years old.
Mark Walters, MD, who recently retired, was one of our most notable practitioners. Dr. Walters was professor and Vice Chair of Gynecology in the Ob/Gyn & Women’s Health Institute at Cleveland Clinic for many years, and was coeditor of Urogynecology and Reconstructive Pelvic Surgery, the main text for the subspecialty with four editions. Along with Mickey Karram, MD, Dr. Walters is thought of as one of the “fathers of urogynecology.” In addition, Tommaso Falcone, MD, currently Chief of Staff, Chief Medical Officer and Medical Director at Cleveland Clinic London, brought advanced laparoscopic surgeries for pelvic floor disorders to the section during his time with us as Chair of the Ob/Gyn & Women’s Health Institute.
I was recruited for the urogynecology section in 1998 to advance our footprint in minimally invasive surgeries. At that time, we were one of the first sections to be approved for a fellowship in Female Pelvic Medicine and Reconstructive Pelvic Surgery, and we graduated our first fellow in the 2000.
Advertisement
Some of our most meaningful accomplishments include the areas of:
Advertisement
Stem-cell and platelet-rich plasma therapies are just now emerging as prospective treatments for pelvic floor disorders, and we are beginning to investigate these therapies at Cleveland Clinic. Microbiome and genetic therapies are also on our radar. Genetic therapies will allow us to discern women who are at risk for incontinence and pelvic organ collapse or collagen vascular disorders, and direct preventative measures or treat patients at an early stage of disease.
Marie Fidela R. Paraiso, MD, is Professor of Obstetrics, Gynecology, and Reproductive Medicine and Vice Chair of Ob/Gyn & Women’s Health Institute at Cleveland Clinic, where she also serves on the Cleveland Clinic Board of Governors. Additionally, Dr. Paraiso holds a joint appointment in the Cleveland Clinic Urological Institute. Her expertise includes laparoscopic and robotic-assisted laparoscopic surgery, urinary and fecal incontinence, pelvic organ prolapse, vaginal surgery and neuromodulation.
She received her medical degree from Indiana University School of Medicine in Indianapolis. She completed her residency in Obstetrics and Gynecology at Good Samaritan Hospital in Cincinnati, Ohio, as well as research fellowships in advanced pelvic surgery and advanced endoscopic surgery and urogynecology at Cleveland Clinic.
Advertisement
Advertisement

Advanced software streamlines charting, supports deeper patient connections

How holding simulations in clinical settings can improve workflow and identify latent operational threats

Interactive Zen Quest experience helps promote relaxing behaviors

Cleveland Clinic and IBM leaders share insights, concerns, optimism about impacts
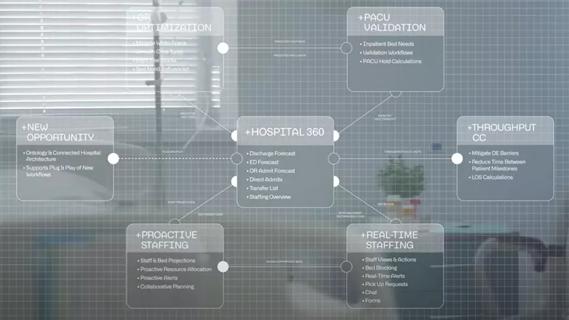
Cleveland Clinic partners with Palantir to create logistical command center

A Q&A with organizational development researcher Gina Thoebes

Cleveland Clinic transformation leader led development of benchmarking tool with NAHQ

Raed Dweik, MD, on change management and the importance of communication