Cleveland Clinic transformation leader led development of benchmarking tool with NAHQ

Quality, safety and data-informed decision-making are hallmarks of modern healthcare. Until recently, however, American hospitals and healthcare systems didn’t have a tool for assessing and evaluating their investment in quality and safety.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Now they do, thanks in large part to Anthony Warmuth, Executive Director of Clinical Transformation at Cleveland Clinic and a board member of the National Association for Healthcare Quality (NAHQ).
In 2021, Warmuth proposed that NAHQ develop a tool that would allow healthcare organizations to benchmark their spending on quality and safety, analyze it over time, and compare their data against peer organizations.
“Cleveland Clinic has a lot of really good infrastructure and sources of data for many disciplines in healthcare,” Warmuth says. “The challenge with quality, safety and patient experience is that each hospital structures their programs so differently. So, it has been hard to benchmark with an apples-to-apples view.”
NAHQ is the preeminent organization dedicated to advancing the profession and discipline of healthcare quality and safety. They are a data-driven resource that sets standards around workforce competencies, workforce planning and development, and quality infrastructure.
Working with a financial benchmarking consultant, leaders from NAHQ, Warmuth and NAHQ members from about a dozen healthcare organizations established what data to include and how to measure it so it would have “enough granularity to be meaningful but not be so detailed as to be burdensome to collect and report,” Warmuth says.
NAHQ offers its Quality and Safety Benchmarking Program to early adopters for a nominal annual fee. Cleveland Clinic participates and has used the tool to help inform budget-making decisions for 2024, Warmuth says.
Advertisement
The current data set includes 15 health systems and 56 hospitals, says Stephanie Mercado, NAHQ Chief Executive Officer.
“We also have another three health systems and 30 hospitals either entering data or about to enter data,” Mercado says. “More are joining monthly, so the number keeps increasing.”
The program establishes a three-year rolling database of financial benchmarks. Organizations pay a single fee regardless of how many hospitals’ data they submit and can generate custom peer groups. Access to the dashboard is unlimited for one year.
Participants start by completing a web-based survey to identify which functions at their organizations are part of the chief quality officer’s domain. Safety and quality functions that do not fall under the chief quality officer are not included. This is a key part of creating relevant comparisons.
“For example, if you have a function called radiation safety, but it falls within a different division, you are not asked to pull data for that,” Warmuth says.
Once the correct functions have been identified, the survey asks for the number of people who serve in each of those functions and the annual expenditure. Relevant outcomes data available from public sources do not have to be manually submitted. For example, CMS Stars rating, Leapfrog scores, hospital-acquired conditions rates and 30-day readmission numbers are obtained from publicly available data.
Once an organization submits its information, it gains access to reporting through a web-based tool that allows comparisons with other hospitals in a variety of ways.
Advertisement
“For example, we can look at how Cleveland Clinic compares to other academic medical centers,” says Warmuth. “Or how we compare to other U.S. News Honor Roll hospitals, or hospitals in the Midwest. So it’s not just a one-and-done report. For financial and staffing benchmarking, it’s very useful.”
As Mercado at NAHQ points out, the tool becomes more useful as more organizations participate. “Continuing to grow the N size is a win for everyone involved,” she says. “More data means more insights to health systems across the country regardless of geography, size, budget or other factors.”
And, adds Warmuth, the need for standardized benchmarking will grow as hospital systems expand their care delivery models.
“Historically, healthcare systems have invested almost all of their quality dollars in the in-patient setting,” says Warmuth. “As more care is delivered beyond the four walls of a hospital – in virtual and ambulatory care settings – we will be better able to track the quality and safety investment in those environments.”
In addition, the financial pressures on modern health systems demand that every dollar be used effectively. “We need to be good stewards of our resources,” Warmuth says. “We owe it to our patients, to our organizations, to our communities and we owe it to our caregivers.”
Advertisement
Advertisement

Advanced software streamlines charting, supports deeper patient connections

How holding simulations in clinical settings can improve workflow and identify latent operational threats

Interactive Zen Quest experience helps promote relaxing behaviors

Cleveland Clinic and IBM leaders share insights, concerns, optimism about impacts
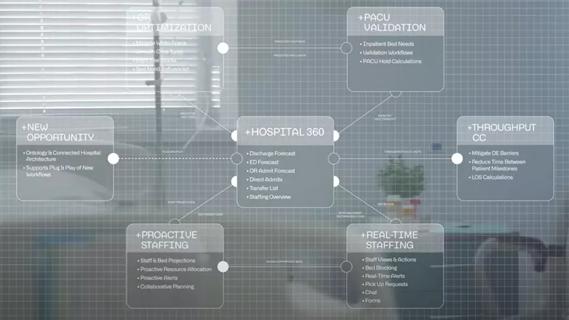
Cleveland Clinic partners with Palantir to create logistical command center

A Q&A with organizational development researcher Gina Thoebes

Raed Dweik, MD, on change management and the importance of communication

Leadership pearls from Margaret McKenzie, MD, hospital vice president