By using free vascularized fascia lata flaps, surgeons can overcome some of the aesthetic and functional challenges historically associated with nasal reconstruction

The nasal columella is one of the aesthetic keystones of the central face, serving as a critical central divider of nasal subunits and providing coverage of critical tip support mechanisms including the lower lateral cartilages and the caudal septum. Reconstruction of defects in this region presents a significant challenge in part due to structural isolation between the lip, nasal tip and nasal airway. This issue is made vastly more challenging when underlying nasal cartilage and septum is also absent. As a result, large defects of the columella have posed a perennial challenge for reconstructive surgeons; despite many described techniques, no ideal solution exists.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Recent innovations with minimal access microvascular techniques and free vascularized anterolateral thigh/fascia lata flaps have allowed complex reconstructions to be performed with near negligible morbidity and vastly abbreviated hospital stays. As a result, indications for these techniques have been extended to more minor reconstructive issues such as facial contour correction, palatal fistula repair, early intervention for osteoradionecrosis and new aspects of nasal reconstruction. A recent article appearing in the American Journal of Otolaryngology-Head and Neck Medicine and Surgery illustrates a new technique for reconstructing columellar and caudal septal defects using vascularized free fascia lata from the anterolateral thigh (ALT) with replacement of tip support structure and concomitant skin grafting. This technique has been employed for isolated columellar defect reconstruction or in combination with the repair of more extensive nasal or lip defects. “When it comes to lesions in the columella, the location and the potential for malignancies to spread to nearby parts of the nose makes the prognosis poorer, so treatments are often more aggressive,” explains Michael A. Fritz, MD, FACS, Section Head, Facial Plastics and Microvascular Surgery in Cleveland Clinic’s Head & Neck Institute and the corresponding author of the study.
He continues, “Patients are often left with ablative defects involving significant cutaneous, nasal lining and structural loss. From a surgeon’s perspective, the nature of these resections have historically posed significant reconstructive challenges. This area of the nose has unique multilaminar and three-dimensional functional architecture. In addition, the paucity of nearby skin, perichondrium, periosteum and mucosa, when septal resection is also performed, magnifies the difficulty of achieving a reasonable functional and aesthetic outcome.
Advertisement
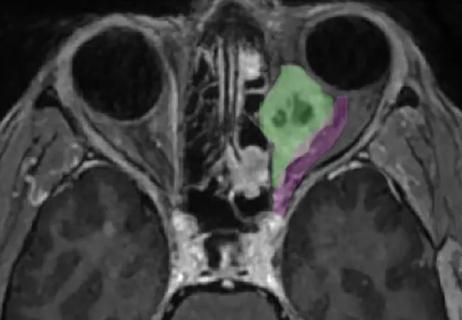
In the described technique, an anterolateral thigh (ALT) flap is harvested with dissection first begun to identify a dominant musculocutaneous or septocutaneous perforator entering fascia lata. A single perforator is typically employed due to the small flap size required. The size of the fascia lata harvested is based on the specific needs of the patient — if, for example, the defect is limited to only the caudal septum and the columella, the flap will measure approximately 4 x 3 cm in size.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/728b9e0a-fced-40f6-843d-e9d63ca8c17d/22-HNI-2851926-FreeVascularzdFasciaLataFlap-TtlColumllaRecnstrctn-CQD-hero_650x450_jpg)
“Despite this being a fascial flap, we include an overlaying skin paddle in the harvest for two reasons,” says Dr. Fritz. “First, it allows for manipulation of the flap without having to worry about damaging the vascular plexus on the fascia lata. The second reason is that it offers substrate for the skin graft to be used as the outer layer of the columellar construct and thus saves the patient the morbidity of a skin graft harvest site.”
In cases where there is extensive loss of cartilage (lower lateral cartilage and caudal septum), harvest of donor cartilage harvest is critical to reestablish nasal tip support and ensure appropriate stability and contour of the columella. This can include use of remaining septal cartilage, along with costal and/or auricular cartilage.
A nasolabial fold incision is used to localize and isolate the preferred recipient vessels — the angular artery and vein. This provides a very aesthetically favorable approach to isolate vessels in close proximity to the reconstruction. Consistent anatomic localization techniques and favorable outcomes with clinical use of these vessels have been previously demonstrated through studies performed at Cleveland Clinic. To accomplish revascularization, the flap is positioned in the central nose and the vascular pedicle is then passed from this location through a subcutaneous tunnel to the nasolabial fold with use of a 5/8-inch Penrose drain. “It’s critical that the flap is harvested as a pure perforator flap to minimize any perivascular bulk and thus allow passage through the tunnel without compression or facial distortion,” says Dr. Fritz
Advertisement
After the vascularized fascia lata has been inset into the defect from the nasal floor and along the posterior septal defect, it is trimmed to size. The structural cartilage that had been previously placed is wrapped with the fascia lata, and grafts are supplemented or modified to achieve a natural-looking nose. After circumferential inset, a split-thickness skin graft attained from the previously removed ALT skin paddle is overlaid. By taking the graft from the paddle, secondary harvest site morbidity may be avoided.
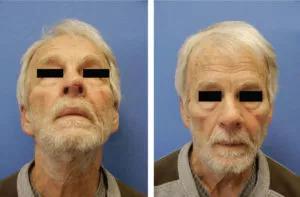
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b323a493-8490-44c9-9080-e3f47004fb25/22-HNI-2851926-FreeVascularzdFasciaLataFlap-TtlColumllaRecnstrctn-CQD-inset_800x525-300x197_jpg)
Post-operative views at 8 weeks. Left: PA
view, Right: worms-eye view .
“When performing nasal reconstruction, there are three critical elements to keep in mind: soft tissue coverage, framework, and internal lining,” says Dr. Fritz. “So in order to achieve optimal columella reconstruction, you need to use something with appropriate skin color, subcutaneous thickness or bulk, width, transition with the tip and external nose, and continuity with the rostral septum and floor. Using free vascularized skin that came from a distant location usually results in a mismatched patch. A free vascularized fascia lata flap overcomes this challenge, as skin grafts on the fascia provide a vastly more favorable color match. Additional benefits of this technique include minimally visible scarring, low morbidity, a relatively predictable contour creation and airway maintenance and, most importantly for the patient, an acceptable aesthetic and functional outcome over time.”
Advertisement
Advertisement

Despite advancements in the specialty, patient-centered care needs to remain a priority

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction

Prompt, multidisciplinary care helps navigate the complexities of a rare condition
Novel collaborative approach helps patient avoid orbital exenteration

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance