EMR alert flags hypercalcemia patients for PTH testing
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7f9f253c-3c3c-4c60-a139-4c8e0433c819/endocrine-system)
endocrine-notes650×340
By Allan Siperstein, MD; Danielle Press, MD; Jamie Mitchell, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Many studies have attempted to determine the prevalence of primary hyperparathyroidism (PHPT). To physicians treating PHPT, the reported prevalence, typically quoted as 0.1 percent, seems to underestimate the number of patients with the disease.
Our study at the Endocrinology & Metabolism Institute confirmed this observation; we found the prevalence of PHPT to be at least eight times higher than previously reported.
We used data from Cleveland Clinic’s electronic medical record (EMR) to assess the prevalence of PHPT and trends in how patients with hypercalcemia are evaluated for PHPT. Our study included 7,269 patients seen over two years (2008-2009) who had hypercalcemia based on at least two outpatient serum calcium levels of 10.6 mg/dL or higher. Our analysis found that two-thirds of these patients were not evaluated for PHPT — even though our assessment determined that 43 percent of patients with hypercalcemia were likely to have the disease.
We presented the results of our study at the American Association of Endocrine Surgeons 34th Annual Meeting, and the research was published in Surgery.
We included only patients who had a primary care physician in our healthcare system to avoid referral bias. Of the 7,269 patients included in the study, only 2,337 patients (33 percent) had parathyroid hormone (PTH) measured based on their hypercalcemic status. The diagnosis of PHPT was documented in the medical records of 95 patients (1.3 percent).
Of the 4,837 patients (67 percent) who did not have PTH measured, we reviewed 200 randomly selected charts for trends in calcium values and the presence of typical comorbidities of PHPT such as nephrolithiasis, osteoporosis, osteopenia or depression, and we looked for alternative diagnoses to explain hypercalcemia, such as multiple myeloma, sarcoidosis or metastatic malignancy.
Advertisement
In our analysis, patients with repeated elevated calcium values and comorbidities suggestive of PHPT were labeled as “likely” to have PHPT.
Patients with alternative explanations for hypercalcemia or a solitary occurrence of hypercalcemia were labeled as “unlikely” to have PHPT.
Of the 67 percent of patients whose PTH was not measured, 28 percent (1,361 patients) were likely to have PHPT. Patients with serum calcium levels greater than 12 mg/dL were less likely than patients with lower calcium values to have PHPT, as other diagnoses such as malignancy were more common among this group.
When we tallied our results from all patients in the study, we found that 57.1 percent (3,476 patients) were unlikely to have PHPT. Of the study population, 9.2 percent had the diagnosis excluded because PTH was low. In those patients who did not have PTH measured, there was not enough evidence in the medical record to support the diagnosis of PHPT, although some of these patients might harbor disease.
The remaining 42.9 percent (3,118 patients) of the study population were likely to have PHPT, although only slightly more than half had PTH measured to make the diagnosis. Of patients likely to have PHPT, very few had the diagnosis documented (1.3 percent of the study population overall) and even fewer were referred for surgery (0.3 percent of the study population overall). Upon our best evaluation of the patients’ charts, 18.7 percent of all patients who were likely to have PHPT did not have PTH testing ordered.
Advertisement
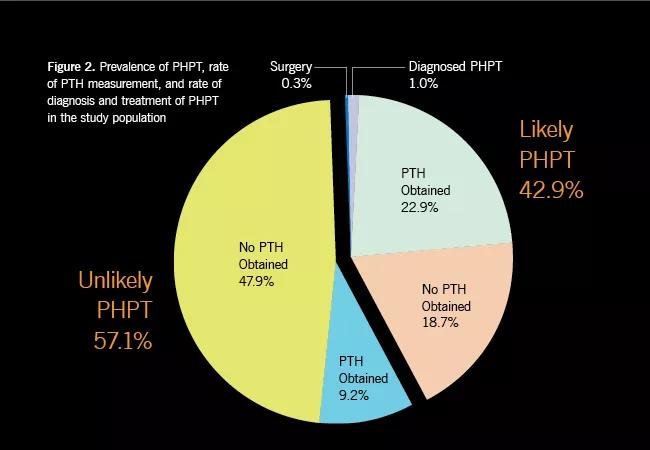
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7f1e4b73-b486-4969-8af6-65aaba537acc/PHPT_650x450_jpg)
We evaluated patient factors associated with having PTH measured. Women, patients with nephrolithiasis and patients with osteoporosis were more likely than their counterparts to have PTH levels checked. However, PTH was measured in only about half of patients with either nephrolithiasis or osteoporosis, even though these diseases are known sequelae of PHPT.
Our study underscores our initial observation that PHPT is more common than previously documented. With the most common cause of hypercalcemia in the outpatient setting being PHPT, we expected to find that most workups for hypercalcemia would include measurement of PTH. Instead, we found that PTH was obtained in only one-third of patients with hypercalcemia.
These findings have been the impetus for the implementation of automated alerts within Cleveland Clinic’s EMR system that prompt physicians to order PTH testing for patients with hypercalcemia. This initiative likely will decrease the incidence of underdiagnosed and undertreated PHPT and is a best practice that could be implemented at other institutions.
Dr. Siperstein is Chair of the Department of Endocrine Surgery, Endocrinology & Metabolism Institute. Drs. Press and Mitchell are former members of the department.
Advertisement
Advertisement
Pheochromocytoma case underscores the value in considering atypical presentations
Advocacy group underscores need for multidisciplinary expertise
A reconcilable divorce
A review of the latest evidence about purported side effects
High-volume surgery center can make a difference
Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D
Patients spent less time in the hospital and no tumors were missed
A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications