Novel assay identifies women most likely to benefit
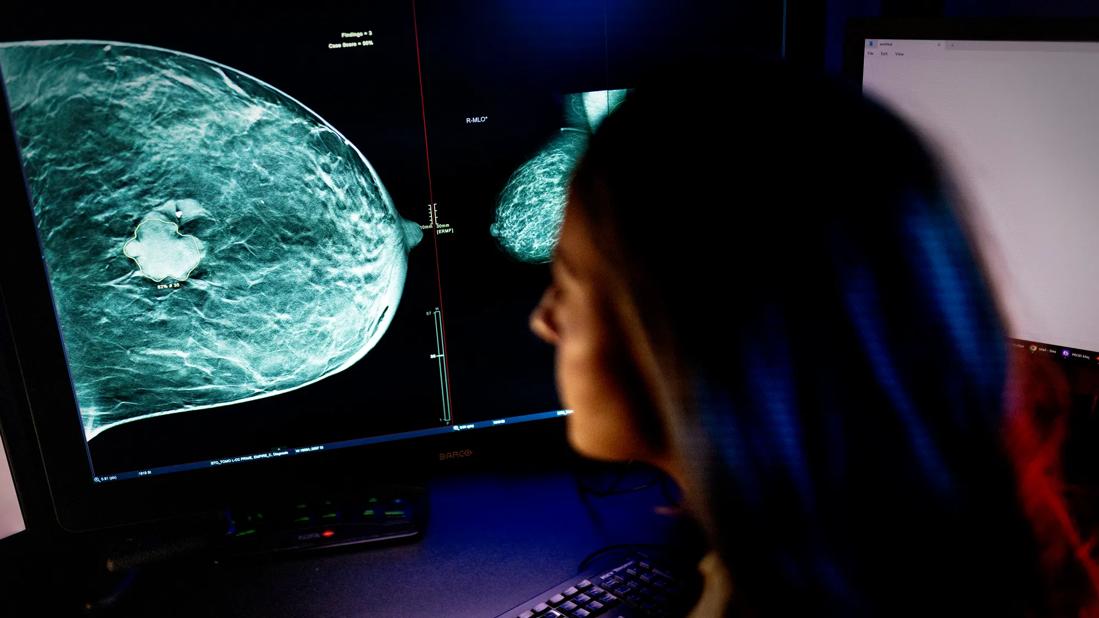
The treatment of ductal carcinoma in situ (DCIS) typically involves breast-conserving surgery followed by adjuvant radiotherapy (RT). Determining whether a patient is likely to benefit from RT or is at low risk of ipsilateral recurrence and could safely forgo the procedure is a clinical challenge, as is identifying those with increased rates of recurrence following standard therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Results from a multi-institutional study led by a Cleveland Clinic researcher, DCSionRT®, a biosignature based on multiple biomarkers, may hold the key to solving that conundrum. The findings were presented Oct. 26 at the American Society for Radiation Oncology (ASTRO) annual meeting.
“With DCSionRT, we identified a high-risk group with two distinct subtypes: patients with a poor response who had high rates of ipsilateral breast tumor recurrence (IBTR) /invasive breast cancer recurrences (IBC) with or without RT, and patients with a good response who derive a significant benefit from adjuvant RT,” explains coinvestigator Chirag Shah, MD, director of Breast Radiation Oncology at Cleveland Clinic.
The research, performed at medical centers in Sweden, Australia and the U.S., involved 250 women with breast tumors larger than 2.5 cm and/or nuclear grade III DCIS who had undergone breast-conserving surgery. Tissue samples from their tumors were tested with DCSionRT, which incorporates p16/INK4A, Ki-67, COX-2, PgR, HER2, FOXA1, and SIAH2.
DCSionRT previously was validated in the SweDCIS randomized clinical trial. Results from that study showed that patients with low-risk DCSionRT DCISionRT scores did not have a significant reduction in the risk of IBTR after undergoing RT. In contrast, high-risk DCISionRT scores were associated with a 9% reduction in risk of IBC if a patient underwent RT.
For the research presented at ASTRO, the authors used Cox proportional hazards and Kaplan-Meier analyses to calculate hazard ratios and 10-year risks of IBTR and IBC, based on DCSionRT scores. IBTR included DCIS or IBC recurrences that were local, regional or metastatic.
Advertisement
Of the women in the study, 72% were classified by biosignature into the high-risk group that was subclassified into those with a good (n = 122) or a poor (n = 57) response subtype. The remaining 28% of women were classified into a low-risk group.
Based on results of DCSionRT, the authors found that the women in the low-risk group who did not receive RT had good 10-year outcomes with no 10-year IBC events, and they derived no significant benefit from RT in terms of 10-year IBTR rates (P = 0.81). In contrast, in the high-risk group, 10-year IBTR/IBC rates (31%/17%) were significantly worse in the women in the low-risk group (p=0.01).
Women in the high-risk group who were treated with RT and had a good response subtype had significantly reduced 10-year IBTR/IBC rates of 5% and 3%, respectively. In contrast, there was no significant benefit with RT among women in the high-risk group with a poor response subtype, who had 10-year IBTR/IBC rates of 25% and 20%, respectively. Patients with a good response subtype had significantly improved outcomes as compared to those with a poor response subtype.
“That is a fivefold higher risk of recurrence for poor response subtype patients than has been documented in the modern literature,” notes Dr. Shah. “To have a 25% rate of local recurrence in the breast after lumpectomy and radiation is unheard of in patients with DCIS based on modern data.”
Reflecting on the strengths and weaknesses of the study, Dr. Shah says the study was relatively small, and while the data were collected prospectively, the analysis was retrospective. However, he notes that the results do add to the limited information available about response to RT among patients with DCIS.
Advertisement
“It was surprising to find that there is a group of patients with DCIS and high-risk features who had a disease subtype that put them at such high risk of recurrence even after lumpectomy and RT,” says Dr. Shah. “The key takeaway for clinicians is to consider using tumor genetics to identify women with DCIS who have a low risk of recurrence that they won’t benefit from RT as well as those that may have higher rates of recurrences.”
He adds, however, that despite those limitations, DCSionRT can be incorporated into clinical practice.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors