Multidisciplinary team tackles complex cases
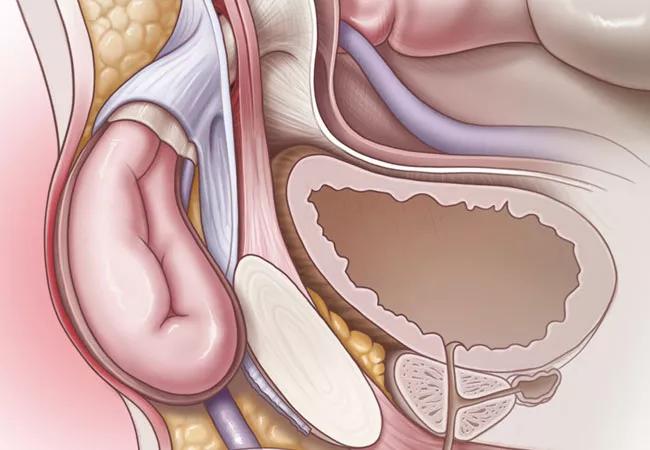
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/856bfe04-e5a5-4b83-a4f0-6f95b301c546/19-DDI-247-Hernia-CQD-Hero_jpg)
19-DDI-247-Hernia-CQD-Hero
A woman from the Pacific Northwest wrote a letter in desperation to Cleveland Clinic general surgeon David Krpata, MD. She had consulted multiple other physicians and was told there was nothing they could do to reduce her severe, chronic pain following inguinal hernia repair.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Krpata invited her to visit Cleveland Clinic’s new Multidisciplinary Chronic Groin Pain Clinic. “She was able to fly in and, in one day, complete her entire evaluation, including imaging and meeting with the surgeon and pain psychologist,” he says.
Her presentation was fairly typical of the patients Dr. Krpata sees at the Groin Pain Clinic. Mesh was placed during her initial hernia repair. She reported pain immediately after surgery, and continued to experience debilitating pain long-term.
After reviewing treatment options, the team recommended she undergo revision surgery — in this instance, mesh removal and a triple neurectomy. After the procedure, “she was pain-free,” Dr. Krpata says.
“She was very thankful,” he adds. “She was in tears – not only because she was pain-free, but also because she had received a thorough evaluation and consideration of her case.”
Cleveland Clinic’s Groin Pain Clinic is one of just a few such facilities in the nation. In addition to treatment, it also conducts research to determine ways to improve outcomes after inguinal surgery and to develop new therapies for chronic groin pain.
Only an estimated 1 to 3 percent of patients who undergo inguinal hernia repair experience debilitating chronic postoperative pain requiring medical attention. Since hernia repairs are common, that small percentage still equates to a large number of people with unresolved pain.
To comprehensively address patients’ chronic pain, the Groin Pain Clinic focuses on 3 Cs: convenience, consultation and individualized care plans.
Advertisement
All medical evaluations take place in a single clinic location and are completed on the same day. “We review everything as a group, including with the radiologist, and come up with a management plan,” Dr. Krpata says. The majority of patients come from out of state, he adds, making the ”one-stop shopping” experience even more important.
The clinic is modeled after a multidisciplinary tumor board, which saves time for clinicians as well as patients. “By design, you get everybody in the same clinic on the same day and it’s easy to get everybody’s input,” Dr. Krpata says. “We don’t have to call or send emails to consultants. It’s direct, it’s done. Then we can call the patient in the afternoon and let them know what our recommendation is.”
Assembling a group of experts to gauge a recommended intervention’s likelihood of success is another distinct advantage of the multidisciplinary clinic, he says. “The more challenging the case, the more input you want.”
Before considering an intervention, the team works to determine the cause of a patient’s groin pain — whether it stems from the previous hernia repair or another cause, such as an injury.
In general, the multidisciplinary team chooses the least invasive intervention first, treating patients in a step-wise fashion when possible. They may start with non-surgical options, such as optimizing the dosage of an existing pain medication, trying other pain medications or, if the pain is neuropathic, using nerve injections delivered by ultrasound neuromuscular radiologists.
Advertisement
Those radiologists can perform a comprehensive groin exam using dynamic ultrasound. “It’s different than the typical inguinal ultrasound,” Dr. Krpata says. “It’s a very thorough, 45- to 60-minute examination of the neuromuscular system of the groin, including the nerves throughout the region and the mesh itself.”
Surgical options include neurectomy (severing the nerve or nerve transection) for neuropathic pain, or mesh removal if the pain is nociceptive as a result of inflammation or scarring around the nerve.
The team’s pain psychologist might recommend reducing medication use, including opioids, prior to revision surgery, while also trying alternative medications such as gabapentin or serotonin and norepinephrine reuptake inhibitors.
Following mesh removal, hernia defects typically are closed with a tissue-based repair. When necessary, new mesh can be placed. Working in proximity to the ilioinguinal, iliohypogastric and genitofemoral nerves and removing the mesh, which becomes encased in scar tissue, is complex and requires specialized training.
“If we can treat the patient without necessarily having to remove their mesh, that would be ideal,” Dr. Krpata says. That’s because mesh removal surgery is not benign. “I always tell patients that putting the mesh in and taking the mesh out are two completely different operations.” Mesh excision creates a higher risk for hernia recurrence in many patients, for example.
“Once the mesh is in and [integrated], you can do damage to the abdominal wall when you take it out,” he adds.
Advertisement
For this and other reasons, treating patients with post-hernia repair pain can be challenging. “Most patients have difficulty finding someone who is willing to manage that situation,” Dr. Krpata says.
“We treat these patients at a high volume,” Dr. Krpata says. “Not every surgeon nationwide has extensive experience treating these complex cases.”
Going forward, Dr. Krpata plans to increase the clinic’s capacity in order to help more people in this population. He also would like to expand services to include additional medical disciplines. “We follow a patient-centered approach,” Dr. Krpata says. “So if we identify modalities that will ultimately benefit our patients, we will try to add them to the clinic.”
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years