May extend disease-free and overall survival with good quality of life
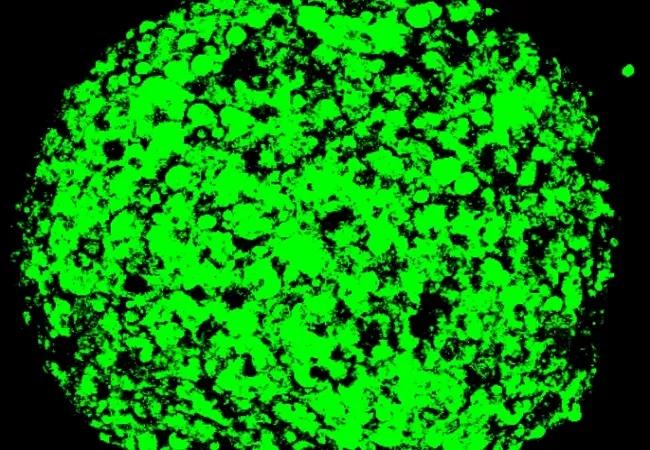
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/28198a24-b438-416b-95ea-8432604aa688/19-CNR-4204-Mesotelioma-case-study-650x450-1_jpg)
19-CNR-4204 Mesotelioma case study 650×450
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 63-year-old woman with prior secondary asbestos exposure was referred to Cleveland Clinic with discomfort in her chest and upper abdomen. Suspicious findings, including right-sided pleural effusion and thickening of the pleura around the effusion, had been detected on chest X-ray, CT scan and PET scan. After further workup, she was diagnosed with epithelioid mesothelioma of her right pleura.
Malignant pleural mesothelioma is an aggressive, often rapidly lethal cancer that requires an individualized, multimodal approach to evaluation and treatment. Because the malignancy pervades the pleura, it is not easily removed surgically. However, patients at Cleveland Clinic Cancer Center who are candidates for a surgical treatment approach typically undergo pleurectomy and neoadjuvant or adjuvant chemotherapy. This approach is not intended to cure the disease but to improve patients’ survival and quality of life. Recurrence is common, most often locally in chest wall areas where the pleura has been removed.
A multidisciplinary team, including specialists in pulmonology, medical oncology, thoracic surgery and radiation oncology, convened to discuss this case. Because of the patient’s relative youth and overall health, the team recommended an innovative combination of extended pleurectomy and chemotherapy followed by pleural intensity-modulated radiation therapy (IMRT). IMRT for mesothelioma is a newer concept that has shown promising results in early studies.
Only 10-15% of pleural mesothelioma patients are candidates for extended (or “radical”) pleurectomy. The patient in this case was recommended for this aggressive surgical approach in part because of the epithelioid histology of her disease. (Epithelioid is the most common and most treatable of the three types of mesothelioma. Disease with sarcomatoid or biphasic histology is associated with shorter survival, so patients tend not to benefit from surgery.) Additionally, the patient had no evidence of metastatic disease according to positron emission tomography scanning and mediastinal lymph node biopsies.
Advertisement
One month after her diagnosis, the patient underwent extended pleurectomy with intraoperative heated povidone-iodine lavage performed by Cleveland Clinic thoracic surgeon Daniel Raymond, MD. The lavage is used in an effort to curb residual micrometastatic disease in areas where the pleura has been removed and to prevent local relapse. Heating the solution increases local absorption and cytotoxic effect. Final pathologic evaluation revealed her tumor to be epithelioid throughout, with areas of extension into the chest wall, staged as pT3N0cM0 disease (Stage IIB).
Following two months of recovery, the patient received four cycles of chemotherapy with a standard regimen of pemetrexed and carboplatin. She then received six weeks of pleural IMRT, directed by Cleveland Clinic radiation oncologist Kevin Stephans, MD.
IMRT is used rather than conventional radiation therapy in order to treat the pleura while sparing healthy lung tissue to preserve function. Twenty-five to 30 daily treatment sessions are needed. Treatment planning is extremely complicated, involving the coordination of hundreds of beams to irradiate the entire pleural surface three-dimensionally around the lung without affecting normal tissue in the lung’s center or adjacent sensitive structures such as the heart, esophagus, stomach, kidney and spinal cord.
IMRT requires complex planning software to calculate precise intensities and angles of radiation beams, and exceptional technical expertise to custom-shape beams for the tumor target. Without skilled planning and image guidance to restrict radiation exposure, this innovative use of IMRT would increases patients’ risk of pulmonary side effects such as pneumonitis, which can be fatal. Techniques such as lung expansion or active breathing control can limit collateral dosage.
Advertisement
Studies suggest lung function declines somewhat over time following treatment. Patients eventually may develop fibrosis or contraction of treated tissue, although functional impairment can be minimized with careful patient selection and radiation sparing of the opposite lung. We have been pleased with the degree of lung functionality our patients have retained to date.
The patient completed her full course of treatment 11 months after diagnosis. Adverse effects included chest pain and shortness of breath after surgery, and low blood counts, nausea and lack of appetite after chemotherapy. She continued to push herself to exercise despite experiencing some weakness and weight loss. She did not require hospitalization for any adverse effects.
Her follow-up care includes computed tomography scans every three months.
Now, 2.5 years since the patient’s diagnosis, her disease remains in remission. There has been no evidence of recurrence on imaging. Considering that mesothelioma has a median survival of 12-16 months, this patient’s outcome is remarkable.
At each follow-up visit, she has shown improved exercise tolerance and increased weight. Her chest pain has resolved completely and her quality of life is excellent.
This case highlights the value of treating pleural mesothelioma with a multidisciplinary approach, including the innovative use of pleural IMRT. Cleveland Clinic Cancer Center is one of few centers in the U.S. that offers this complete treatment package to appropriate patients.
Advertisement
Adding pleural IMRT to surgery and chemotherapy — even without curative intent — may contribute to better outcomes and longer remission in patients who are willing to accept the increased toxicity risk. This aggressive treatment can be administered effectively and with manageable side effects.
Unfortunately, most patients with mesothelioma are not candidates for multimodal treatment due to age, comorbidities and disease histology. However, it is worth investigating through referral of newly diagnosed patients to an experienced mesothelioma team.
Dr. Stevenson is Vice Chair of Hematology and Medical Oncology at Cleveland Clinic Cancer Center.
Feature image: Three-dimensional image of a mesothelioma spheroid.
Credit: National Cancer Institute Center for Cancer Research
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches