Rare pregnancy complication can lead to fetal demise
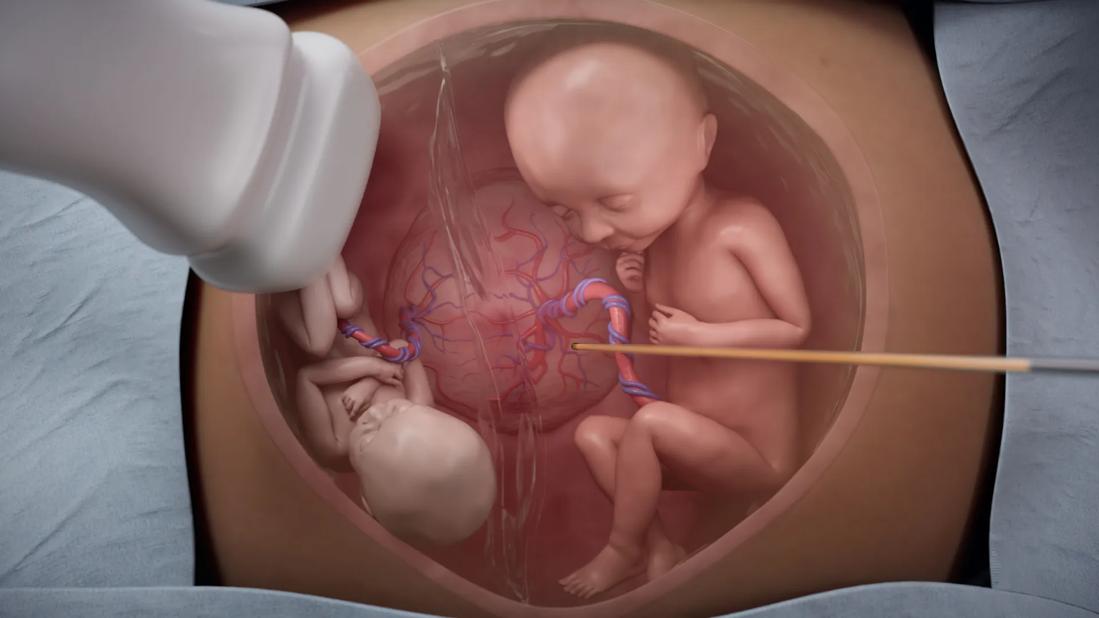
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2aba0d19-235c-4a09-967c-8d5425cc634b/twin-transfusion-case-study)
Illustration of small and large fetuses in patient with twin to twin transfusion syndrome
A 28-year-old woman in her second trimester carrying monochorionic twins was receiving care from Cleveland Clinic’s Maternal-Fetal Medicine team. During an ultrasound, Maeve Hopkins, MD, noted an amniotic fluid discordance between baby A and baby B and was concerned about possible twin-twin transfusion syndrome (TTTS; sometimes called twin-to-twin transfusion syndrome). She referred the patient to Courtney Stephenson, DO, director of fetoscopic intervention at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Stephenson met the patient days after the ultrasound and diagnosed her with stage 2 TTTS with severe growth restriction. The following day she performed fetoscopic laser ablation to arrest the intertwin transfusion.
“If left untreated in severe, early-onset cases, twin-to-twin transfusion has an 80% to 100% mortality rate,” says Dr. Stephenson. “Survival rates for one or both babies who undergo the fetoscopic procedure are about 90% to 92%.”
TTTS is a problem of placental development that occurs in approximately 10% to 15% of monochorionic twin pregnancies and causes an imbalanced blood flow between the babies. The donor twin receives less blood flow from the placenta and becomes hypovolemic. Conversely, the recipient twin receives too much blood and becomes hypervolemic.
“It’s a dynamic of one baby being under-perfused and the other one being over-perfused,” says Dr. Stephenson. “The twin that gives blood away becomes dehydrated, its kidneys can shut down and on ultrasound we may no longer see a bladder. The recipient twin is generally larger with volume overload, placing the heart under significant pressure, and this can lead to cardiac dysfunction.”
The severity of TTTS, which can develop at any point in a pregnancy, is assessed using the Quintero Staging System:
Advertisement
Fetoscopic laser ablation is a causative therapy that has been shown to be the best first-line treatment for TTTS. It can be performed between 16 and 26 weeks gestation from stages 2 through 4. Patients are awake during the percutaneous procedure and receive a spinal epidural. A trocar and cannula are inserted through the skin and directly into the uterus under ultrasound guidance. Ideally, the fetoscope is inserted in the recipient twin’s overdistended amniotic sac to avoid septostomy and facing the vascular equator.
After the surgeon identifies, maps and names all the unpaired vessels on the surface of the placenta, the surgeon performs laser coagulation of the abnormal placental anastomoses to stop the abnormal unbalanced blood flow and then drains redundant amniotic fluid.
When Dr. Hopkins performed the ultrasound on the patient in July 2024, there was a fluid discordance — 2.5 cm in the donor twin and 7 cm in the recipient twin, below the Quintero Staging criteria.
Just days later, Dr. Stephenson met with the patient. Ultrasound revealed the donor twin had almost no fluid (0.6 cm) while the recipient twin had >10 cm.
“She was diagnosed with severe intrauterine growth restriction (IUGR),” says Dr. Stephenson. “Baby A was small — less than tenth percentile — and the bladder was not visible. The babies had stage 2 twin-to-twin transfusion syndrome.”
The patient underwent fetoscopic laser ablation at 21 weeks gestation, and the results were excellent.
“Baby A had a full bladder the next day,” says Dr Stephenson. “Six days post-op, the smaller IUGR baby had totally normal fluid and normal Doppler studies.” The patient was followed closely twice weekly until delivery.
Advertisement
Twins with TTTS are monochorionic diamniotic. However, after the procedure it became apparent that the dividing membrane had broken down in one area. A post-operative visit revealed that the twins in this case were partially monoamniotic.
“The membrane was intact between the babies’ heads, but when you got down to their legs, the babies were in the same space,” says Dr. Stephenson. “The umbilical cords were getting tangled, so we admitted the patient to the hospital for observation to ensure the cords didn’t knot.”
The patient was closely monitored in a high-risk unit for four weeks, then delivered by Caesarean section at 32 weeks gestation.
“The twins were both delivered at the same time because they were in the same sac,” says Dr. Stephenson. “They have the exact same birthday by year, month, day and minute.”
Dr. Stephenson has been performing fetoscopic laser ablation procedures for advanced TTTS since 2010. She offers observations on four areas related to the surgery:
Advertisement
Before joining Cleveland Clinic in 2023, Dr. Stephenson opened two other fetal care centers in the U.S. She admires patients confronted with a TTTS diagnosis.
“Taking care of these women is quite profound. They do not need surgery. They are fine. Yet they put themselves on an operating table for the sake of babies they have never seen or held,” says Dr. Stephenson. “I am very moved by the universal strength and courage of mothers. These women who choose fetoscopic laser surgery are heroes.”
Advertisement
Advertisement
Blood test along with ultrasound is beneficial for twin pregnancies
Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence
Least-invasive open-heart AVR option to date yielded rapid recovery in all cases
First single-port renal vein transposition reduces recovery time and improves outcomes
Approach offers a ‘middle ground’ between radical prostatectomy and active surveillance
The low anterior access approach using the single-port robot is gaining attention within the field
Research may offer family-planning insights for those with the condition
Largest study examines factors affecting asthma exacerbations during and after pregnancy