Study shows encouraging safety results in rare type of adult brain cancer
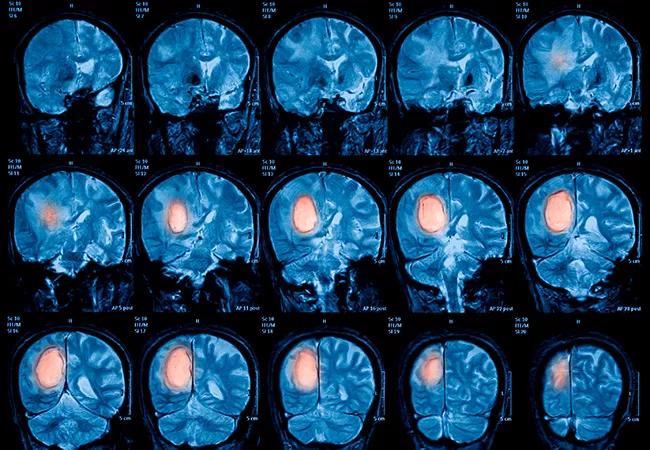
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/531b5d31-5914-46f9-a1ff-381926b0452c/21-CNR-2409162-CQD-650x450-1_jpg)
Magnetic resonance imaging (MRI) of the brain, brain tumor
A study conducted in 22 adult patients with low-grade glioma found that concurrent temozolomide-based chemoradiation therapy does not adversely influence neurocognitive function during a 2-year treatment follow up. Cleveland Clinic investigator Erin S. Murphy, MD presented the early findings of this collaborative research at the American Society for Radiation Oncology (ASTRO) 2021 Annual Meeting held in Chicago on October 24-27, 2021.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Cognitive function remained stable following combination therapy in our patient population, which is good news,” she says. “It is really nice to be able to let [the patients] know that, in the setting of combined treatment to try and stop their tumor from growing and progressing, there doesn’t seem to be a significant impact on these prospectively evaluated neurocognitive endpoints.”
In explaining the rationale behind this work, Dr. Murphy notes that low-grade glioma patients are heterogenous and can have longer-term survival (14+ years) and a more indolent course over time, which makes it particularly important to study the impact of therapies on overall quality of life and cognitive function.
“We have been treating patients for a while in the same way — all of our low-grade glioma patients receive radiation with concurrent chemotherapy, temozolomide, followed by adjuvant temozolomide,” she says, “but there hasn’t been much data published about the impact of this specific combination therapy on neurocognitive outcomes.”
The study included 22 adult patients with low-grade glioma treated with concurrent radiotherapy and temozolomide at Cleveland Clinic between 1980 and 2020. Neurocognitive testing was done prior to and after treatment. According to Dr. Murphy, the study focused on adult patients only because low-grade gliomas in adults are driven by different molecular features than those in children, and the impact of treatment would also likely be different in younger patients.
Advertisement
54 Gy was delivered in 30 fractions to most patients, and the temozolomide regimen consisted of a daily dose of 75 mg/m2 given concurrently during the radiotherapy followed by an adjuvant dose of 150-200 mg/m2 given on days 1-5 every 28 days. Cognitive testing was performed in all participants and focused on assessing several areas of neurocognitive function, including verbal memory, executive function, visuospatial memory, semantic and phonemic fluency, processing speed and naming. After receiving a baseline cognitive evaluation, patients were also evaluated at several different points post treatment.
Although the mean test scores of most assessments were slightly lower at follow-up evaluation compared to the baseline, the changes were not significantly different, indicating essentially stable cognitive function after treatment. When looking across the different neuropsychological assessments, a decline in performance was observed only in 3 patients (16.7%) and an improvement was observed in 2 patients (25%).
“Depending on risk factors, some patients may initially be observed following surgery. However, once we recommend treatment, it is really helpful to be able to offer what we have learned about neurocognitive impact of our treatment with our patients,” she says.
In terms of the clinical impact of these findings, Dr. Murphy notes that they can help inform the discussion between patients and their providers around the risks and benefits of treatment. However, additional studies are still needed to better understand the long-term impact of treatment on neurocognitive function in patients with low-grade glioma.
Advertisement
“We still need longer term follow-up, knowing that these patients will survive much beyond the timepoint of evaluation in this study, and [we should] include these neurocognitive endpoints on prospective trials so that we can continue to follow them over time and understand the later impact better,” she says.
Another important thing to examine, she adds, is any correlation between neurocognitive outcomes and radiotherapy dose to certain sensitive regions of the brain.
“Sometimes there can be a correlation between brain anatomy and neurocognitive outcomes in patients,” she says. “We can now go back and look at our radiation plans and examine the dose [delivered] to certain critical structures like the hippocampus or the temporal lobe, and try to assess whether there is a dose relationship that correlates with these neurocognitive outcomes as well.” Dr. Murphy’s team is currently in the planning stages of this research.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches