Even high-risk patients see long-term benefit
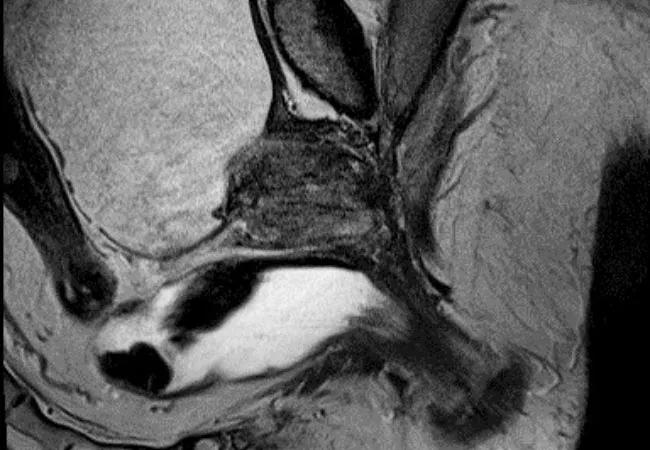
Brachytherapy for prostate cancer is one approach at Cleveland Clinic for patients with localized prostate cancer. Jay Ciezki, MD, radiation oncologist in Cleveland Clinic’s Glickman Urological & Kidney Institute, hopes widespread adoption of the modality is on the horizon.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This is a proven, convenient treatment method for patients with localized disease,” says Dr. Ciezki. “We’ve shown that low- and high-dose brachytherapy works as monotherapy or in combination with other treatment methods for a variety of prostate cancer types, and I think all discussions of definitively managed prostate cancer treatment should include brachytherapy.”
Cleveland Clinic researchers and clinicians have published dozens of peer-reviewed articles demonstrating the safety and efficacy of brachytherapy, including a 2018 study published in JAMA that established that the addition of brachytherapy to high-risk prostate cancer treatments improved survival outcomes. Recent research led by senior author Rahul Tendulkar, MD, Department of Radiation Oncology, validated the prognostic utility of the National Comprehensive Cancer Network’s 2019 risk stratification subgroups for men treated with brachytherapy.
“Both the clinical and research sides of our prostate brachytherapy program are very robust,” says Georges-Pascal Haber, MD, PhD, Interim Chairman of Glickman Urological & Kidney Institute. “We also are able to translate the convenience of the modality itself to the patient experience. We complete preoperative testing, treatment and postoperative follow-up in a three-day period.”
In September 2021, the program will reach a new milestone – 25 years since the first patient was treated at Cleveland Clinic. To date, over 6,200 patients have been treated with brachytherapy at Cleveland Clinic main campus, and that number continues to grow.
Advertisement
Prostate cancer remains the most commonly diagnosed non-skin malignancy in American men and, despite earlier detection and advances in treatment, it is still the second-leading cancer-related cause of death. High-risk prostate cancer affects 7 to 10 percent of men with the disease and is the most difficult form to treat. “We don’t see many centers treating high-risk patients with brachytherapy,” says Dr. Ciezki, “but our research and outcomes show that it should definitely play a role for appropriate patients.”
A 2016 study published in the International Journal of Radiation Oncology, Biology and Physics examined over 2500 high-risk prostate cancer patients treated at Cleveland Clinic and found that patients treated with low-dose-rate brachytherapy (LDR) and external beam radiation (ERBT) improved biochemical recurrence-free survival compared with radical prostatectomy (RP). Patients who received LDR or RP saw lower prostate cancer-specific mortality than those treated with ERBT. Overall, LDR was least toxic to patients.
Cleveland Clinic tracks and publicly reports outcomes as part of its commitment to transparency and quality improvement. In 2018, of 963 patients with high-risk prostate cancer, the 352 patients treated with LDR showed a 15-year cumulative mortality of 5.7% compared with 18.9% for patients treated with ERBT (see more details here).
Brachytherapy is an option for even high-risk patients, but it’s not for everyone. “The literature shows that patients with bladder obstruction issues and extremely advanced localized cancer would be better served with other treatment options,” says Dr. Ciezki. “But for patients considered low or intermediate risk, and even some patients with larger prostate size or considered high risk, physicians should consider brachytherapy as an effective therapy or complement to therapy that can potentially improve outcomes and decrease toxicity.”
Advertisement
Advertisement

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists