How a multicenter consortium aims to change the research landscape
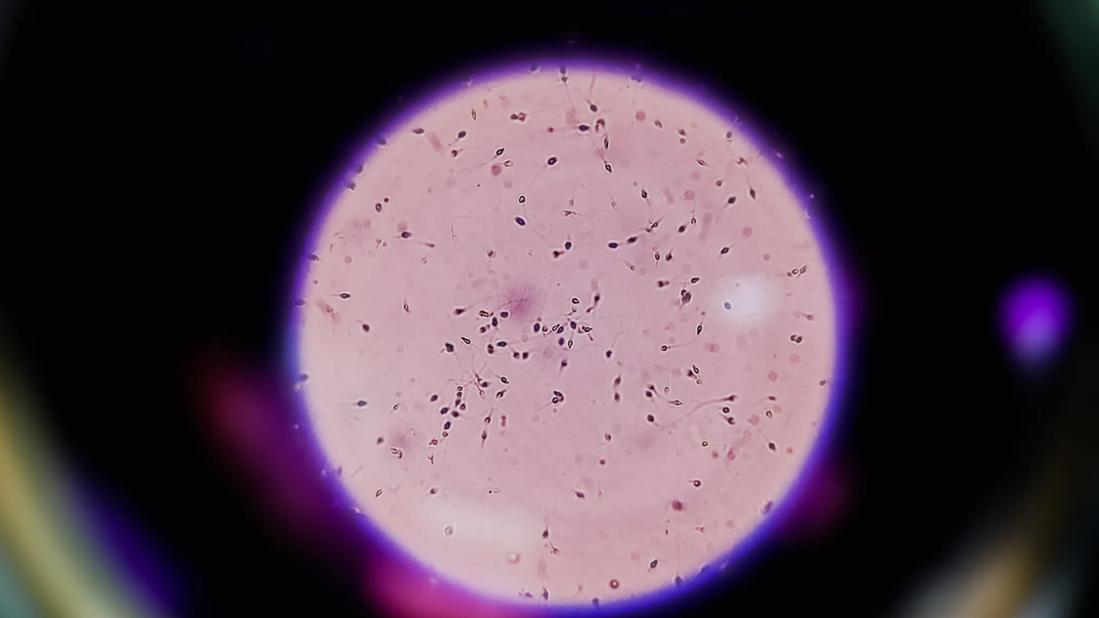
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8a849cb7-6de6-45de-a4fc-cf0c8eae2d0f/sperm-analysis-on-microscopic-examination-1894889861)
Sperm analysis on microscopic examination
A multi-institutional consortium called MOBY.US (Male Organ Biology Yielding United Science) is combining forces and sharing data to advance the robustness of research into male infertility.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Launched in 2023 by Cleveland Clinic urologist and male fertility specialist Scott Lundy MD, PhD, the collaboration now comprises 14 centers, over 50 physicians, and more than 5,000 patients. Those numbers are all expected to increase over time. The consortium has published three papers thus far and have presented several abstracts at medical conferences.
Male factors contribute to at least half of infertility cases, yet research into male infertility has lacked statistical rigor. “Many of the studies in male factors in fertility are done at one hospital with a small group of patients in a retrospective manner and draw conclusions from small numbers of patients. We know that science conducted in that way is not as sound as it could be,” Dr. Lundy says.
So, he and other male infertility experts around the country put together a consortium of large hospitals and academic centers to work together to improve the clinical relevance of the research. “We've created a standardized, very robust system for collecting data, with about 400 data points per patient, and sharing those data across institutions,” Dr. Lundy says.
The name “MOBY.US” is a nod to both to the sperm whale of novel fame, Moby Dick, as well as the Mobius strip, representing perpetuity.
Currently, the consortium has an outward-facing website as well as an internal site for data sharing. They’ve obtained data use agreements from the participating institutions, many of which have secured Institutional Review Board approval for their work.
Advertisement
Their approach is democratic. “There is no one lead on a study, but rather we all have equal say and equal ability to guide the questions that are being asked, and all groups who participate have access to all of the data, as long as they're actively participating,” Dr. Lundy explains.
The ultimate goal, he says, “is to have rare populations where a single center might see three to five patients over a decade with a certain condition, and if ten institutions contribute their five patients, then suddenly this becomes a much more important group that can answer more clinically relevant questions. Conversely, we can add 10,000 patients or 20,000 patients with common conditions like general infertility, or varicocele, and ask similar questions, but have much more important and robust answers.”
Thus far, they’ve published Testosterone and luteinizing hormone predict semen parameter improvement in infertile men treated with anastrozole in October 2023 in the journal Fertility and Sterility, and Combination clomiphene citrate and anastrozole duotherapy improves semen parameters in a multi-institutional, retrospective cohort of infertile men in February 2024 in Translational Andrology and Urology.
And in December 2023, consortium members penned an editorial with the compelling title Deafening Silence of Male Infertility, aiming to enlighten readers about the human side of infertility, with patient voices of those who have struggled with it. It concludes with “a glimpse into the future of research and experimental technologies to provide hope in treatment options.”
Advertisement
There’s much more to come. Members have spoken about the consortium at the 2024 meetings of the American Society for Reproductive Medicine and the Sexual Medicine Society of North America. They have now submitted several abstracts to the upcoming American Urological Society meeting to be held April 26-29, 2025 in Las Vegas.
While the consortium will initially collect high-quality retrospective data, “ultimately, the goal down the road is to flip the switch away from retrospective studies and start doing prospective randomized control trials as a gold standard for data and for decision making. That's in the works, but it takes time. We’ve started to think about what those projects might be, but we need funding and buy-in and trust,” Dr. Lundy explains.
As yet, there is no funding. “This is all a labor of love by the reproductive urologists who lead these efforts. We will be seeking funding from many institutions.”
Advertisement
Advertisement
Reproductive urologists publish a contemporary review to guide practice
Sperm counts haven’t declined among American men in recent years, new research from Cleveland Clinic finds.
Male factors play a role in about half of all infertility cases, yet men often are not evaluated
Findings expand upon earlier data, providing new noninvasive options
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
American Urological Association presentation outlines the latest evolution of treatment protocols
Early, individualized diagnosis and comprehensive management key to preserving fertility
Surprise findings argue for caution about testosterone use in men at risk for fracture