An old drug shows new promise for a rare childhood cancer
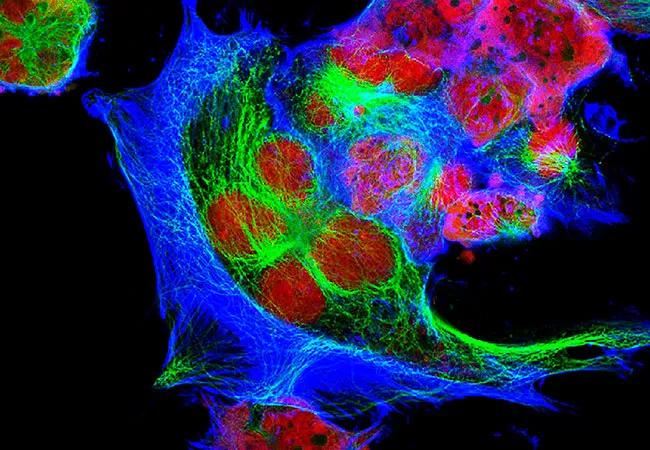
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5df4048e-909d-4258-86cc-13c9a2ffcfcb/650x450-Neuroblastoma-jpg)
Zahler, DO
Neuroblastoma affects approximately 800 children in the U.S. each year and accounts for about 6% of all childhood cancers. Unlike intermediate- or low-risk forms of the disease, which have a relapse rate of about 5% to 15%, high-risk pediatric neuroblastoma carries a 50% to 60% risk of recurrence or resistance to therapy. Perhaps due to the unavailability of effective post-treatment maintenance therapy, a large fraction of patients with high-risk neuroblastoma relapse within the first five years of treatment completion.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Neuroblastoma is really a spectrum of disease,” says Stacey Zahler, DO, a pediatric hematologist/oncologist with Cleveland Clinic Children’s. “A patient can have neuroblastoma or even metastatic disease at birth, and treatment might not be necessary because the tumor cells will regress over time. On the other end of the spectrum is a very aggressive cancer that is very difficult to treat and requires all treatment modalities, including intensive standard chemotherapy, an aggressive surgery, radiation and immunotherapy, and one or two autologous stem cell transplants in between surgery and radiation.”
Beat Childhood Cancer (BCC), a collaborative research consortium that brings together more than 40 universities and children’s hospitals across the U.S., is now trying to change the course of this serious illness by exploring the potential of an old drug, difluoromethylornithine (DFMO), to prevent neuroblastoma recurrence in patients who have achieved complete remission (CR) after completing standard therapy.
“DFMO is an irreversible inhibitor of ornithine decarboxylase [ORD], an enzyme involved in the synthesis of polyamines in the body,” explains Dr. Zahler. “It was originally approved by the FDA in high doses to treat West African sleeping sickness. Research in Giselle Sholler’s laboratory at Helen DeVos Children’s Hospital in Grand Rapids, Michigan, has shown that neuroblastoma cells have a high polyamine content and high levels of ORD, so universally inhibiting ORD is a way of targeting tumor cells.”
Advertisement
In a phase 2 trial published recently, Dr. Sholler’s group showed that DFMO is effective in patients with high-risk neuroblastoma, increasing event-free survival at two years post-treatment by at least 20% to 25%.
In the scope of BCC, Dr. Sholler is now leading an expanded, confirmatory phase 2 trial to study the effectiveness of a 730-day treatment course of oral DFMO in pediatric and young adult patients with neuroblastoma who have achieved a complete remission (CR). Cleveland Clinic joined BCC in 2018, and Dr. Zahler is principal investigator at Cleveland Clinic Children’s for this multicenter trial, which is enrolling patients across 26 states.
The study’s purpose is to assess the utility of DFMO as a single-agent prevention strategy for neuroblastoma recurrence. The trial is divided into four strata based on patients’ disease history and past treatments and is part of the larger effort to get DFMO approved by the FDA for treatment of neuroblastoma.
“The first stratum is for patients who are in CR after completing the standard COG [Children’s Oncology Group] therapy,” Dr. Zahler explains. “The second stratum is for patients who are in CR after completing the standard European protocol therapy or other type of first-line treatment protocol. The third stratum is for patients who are in a first remission after receiving additional treatment for refractory disease, and the fourth stratum is for patients who had a relapse and achieved CR following a relapse. Trial inclusion criteria are a pathologically confirmed diagnosis of high-risk neuroblastoma, age less than 31 years and a negative I-123 MIBG (metaiodobenzylguanidine) scan as confirmation of CR.”
Advertisement
In the study, DFMO is given twice a day for 27 four-week cycles (2 years), with the dose (from 500 to 1,000 mg/m2 twice daily) based on the patient’s body surface area. At the time of writing, Cleveland Clinic was enrolling patients in all four strata.
“We [the BCC consortium] are now close to our accrual goal of 92 subjects for strata 1 and 2 and 35 subjects for strata 3 and 4, but we will likely continue to enroll patients because this drug has been so effective,” Dr. Zahler notes.
Dr. Zahler says the preliminary results are promising and she is optimistic about DFMO’s effectiveness in the maintenance setting.
“Over the decades we have really made advancements in overall survival of patients with neuroblastoma, but I believe DFMO has the potential to allow a much larger number of patients to survive,” she says. “Additionally, its side effect profile is minimal and usually includes skin rashes and brittle hair. Only about 4% of patients in the studies had evidence of hearing loss, which was completely reversible after stopping DFMO treatment.”
Dr. Zahler says the next step after completing this phase 2 trial is to test DFMO in a phase 3 trial and seek FDA approval.
“We are well on our way there and are hopeful that DFMO may get approved sooner than the standard 12 years that approvals typically take,” she says. “Sometimes drugs can obtain FDA approval after a very successful phase 2 trial, and this is our hope for DFMO.”
Image at top shows human neuroblastoma cells.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches