Meta-analyses signal an opportunity to reshape risk stratification and surgical protocols for these comorbidities
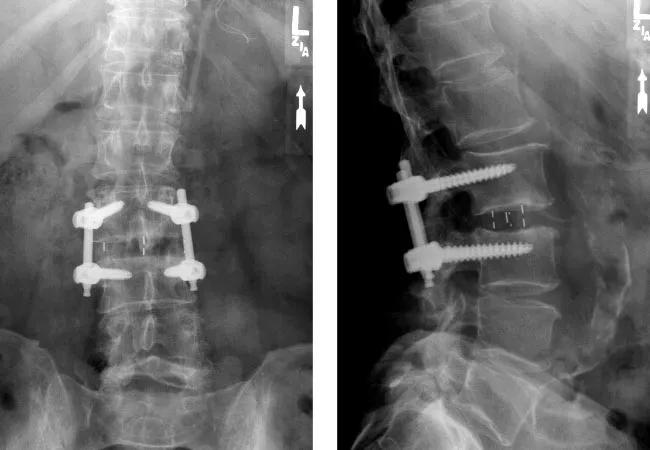
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0c7edca2-4313-43e2-a3ec-cf32ab720bdb/19-NEU-5571-lumbar-interbody-fusion-650x450-jpg)
x-rays of hardware between spine segments
Two recent systematic reviews and meta-analyses underscore a key message for spine specialists: diabetes and obesity significantly compromise outcomes following spinal fusion surgery. The analyses, which collectively evaluated data from 180,000 patients, revealed increased risks of nonunion and worse patient-reported outcomes in individuals with these conditions who underwent spinal fusion.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The findings have important clinical implications, as almost 80% of lumbar fusion patients in the United States have obesity and the current 15% to 25% prevalence of diabetes among spinal surgery patients is expected to increase by 35% by 2045.
“As prevalence rates of diabetes and obesity continue to rise globally, understanding these conditions’ impact on spine surgery outcomes is paramount for optimizing patient care and resource allocation,” says spine surgeon Michael Steinmetz, MD, Chair of Neurosurgery at Cleveland Clinic and a co-author of both analyses. “Spine surgeons will likely find these results helpful for risk stratification, surgical planning and postoperative management.”
Both papers were published in Spine (2025 Epub 19 May and 2025 Epub 28 May) by a team of co-authors from nine centers in the U.S., Canada and Spain.
Diabetes mellitus and obesity have long been suspected of impacting orthopaedic surgical outcomes due to their systemic effects. Previous research on the specific relationship between these conditions and spinal fusion success, particularly nonunion rates and patient-reported outcomes (PROMs), has been inconsistent or limited. “We undertook these analyses to consolidate the evidence to date and seek clearer insights,” Dr. Steinmetz explains.
The mechanisms by which diabetes and obesity may impair spine fusion healing and recovery are complex. Diabetes can lead to microvascular compromise, endothelial dysfunction and impaired blood flow, which are crucial for bone formation and remodeling at the fusion site. The disease also can hinder bone metabolism by disturbing the balance between bone formation and resorption. In the setting of obesity, excessive mechanical loading on implants, metabolic factors like vitamin D deficiency, and potential lower bone mineral density may contribute to nonunion. Both conditions are associated with chronic pain and inflammation, which can further complicate postoperative recovery and undermine quality of life.
Advertisement
The two studies were conducted as systematic reviews and meta-analyses, adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The authors conducted systematic searches across major electronic databases including PubMed, EMBASE, Scopus and Cochrane Library, imposing no date or language restrictions to ensure broad inclusion of relevant investigations, which were all comparative (cohort or case-control) studies.
This meta-analysis included 18 studies with a total of 118,617 patients, comparing outcomes among patients with and without diabetes who underwent spine fusion surgeries. Outcomes of interest were the incidence of spinal pseudoarthrosis (nonunion) and PROMs, including scores on a visual analog scale (VAS) for pain, the Oswestry Disability Index (ODI), the EuroQol-5D (EQ-5D) and short-form surveys (SF-12/36).
This meta-analysis focused specifically on lumbar spinal fusion, including 15 studies with 61,341 patients comparing outcomes between those with obesity (body mass index [BMI] ≥ 30) and those without it. Primary outcomes were the incidence of spinal nonunion, PROMs (ODI, VAS, SF-12/36), and associated healthcare costs.
In the diabetes analysis, patients with diabetes had a significantly higher incidence of nonunion at the lumbar spine (odds ratio [OR] = 1.13; 95%CI, 1.02-1.25; P < .05). Notably, no significant difference was found at the cervical level, which the authors speculate may be due to the cervical spine’s greater structural resistance, lower biomechanical stress and superior vascularization relative to the lumbar region.
Advertisement
In the obesity analysis, obesity was associated with a more than twofold increase in risk of nonunion following lumbar spinal fusion (OR = 2.10; 95%CI, 1.23-3.60; P < .01). This finding remained robust even after sensitivity analyses.
Both conditions were consistently linked with worse PROMs, indicating higher pain and disability.
In the diabetes analysis, patients with diabetes reported increased VAS back/neck pain scores at both the cervical and lumbar levels; worse ODI outcomes, indicating greater disability; and worse quality of life as measured by EQ-5D and SF-12/36 scores. While the mean differences were statistically significant, they often fell short of minimally clinically important difference (MCID) thresholds for VAS, ODI and EQ-5D scores, although some MCID thresholds for SF-36 scores were met. “This highlights a potential area for further research into the clinical meaningfulness of these statistical differences,” Dr. Steinmetz notes.
In the obesity analysis, patients with obesity reported significantly worse ODI scores, greater pain as measured by both VAS back and leg pain assessment, and significantly worse SF-12/36 scores. MCID was not assessed in enough studies for comprehensive analysis.
The obesity analysis found that obesity was associated with significantly higher hospitalization costs (P < .001), which aligns with previous findings on increased hospital costs in surgical patients with obesity. Economic effects were not analyzed in the diabetes analysis.
Advertisement
The author team behind these meta-analyses notes that their findings provide compelling evidence that spine specialists must proactively address diabetes and obesity in patients undergoing spinal fusion. They recommend the following:
Advertisement
Despite the large patient samples included in these meta-analyses, the authors note that their findings do not definitively establish direct causality due to the recognized limitations of such analyses, including the included studies’ predominantly retrospective cohort designs and lack of heterogeneity among study protocols. They call for high-quality prospective studies to further delineate the isolated effects of diabetes and obesity on spinal fusion outcomes, including better assessment of MCID thresholds.
“Nevertheless, these findings reinforce the advisability of comprehensive preoperative evaluation, proactive comorbidity management, tailored surgical planning and robust postoperative care to improve outcomes in the increasing segments of spinal fusion patients with diabetes or obesity,” Dr. Steinmetz concludes.
Advertisement
Success for these complex operations requires judicious patient selection and presurgical patient optimization
Minimally invasive approach is gaining prominence as a fast and safe outpatient procedure
A preview of Cleveland Clinic’s emerging AI platform for spine care decision-making
Findings could help clinicians make more informed decisions about medication recommendations
The advanced stage of diabetic retinopathy is among the most challenging for retinal surgeons
Association revises criteria for the diagnosis and resolution of severe conditions
Consider each patient's unique disease progression and treatment goals when choosing a strategy
While results were negative for metformin, lifestyle counseling showed surprising promise