Accurate, transparent documentation may reduce risks associated with common disorder
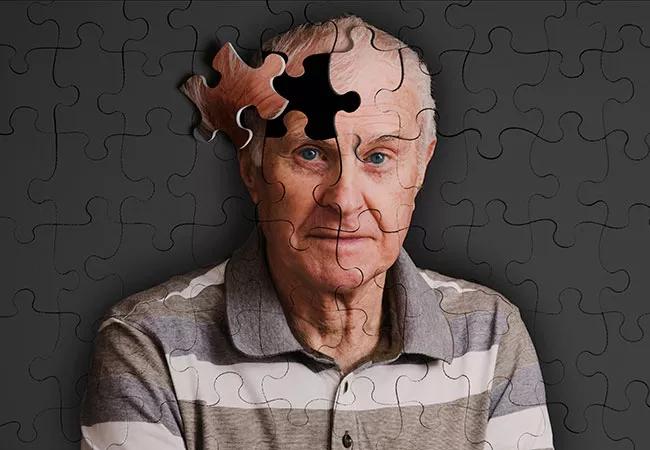
Delirium, a common disorder in hospitalized geriatric patients, often heralds poor short- and long-term outcomes. Evidenced by an abrupt change in mental status, the disorder can result in increased length of stay and other complications, including permanent cognitive impairment. Despite its prevalence and substantial risks, however, delirium often goes unrecognized in hospital and post-hospital settings alike.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Delirium is especially problematic for individuals who already have an underlying cognitive impairment or dementia,” explains Ronan Factora, MD, a physician and researcher in the Center for Geriatric Medicine at Cleveland Clinic. “It’s not unusual for these patients to have trouble bouncing back to where they were before the onset of delirium. As a consequence, they may become more cognitively and functionally impaired, and require a lot more help at home.”
A new project led by Dr. Factora aims to better the outcomes of patients with acute confusion by refining the quality and consistency of their hospital records. Determined to further improve how clinicians diagnose and manage delirium, his team is taking advantage of a digital dementia dashboard used to streamline care and reduce risk.
Information from electronic health records, including delirium screening results and order sets, are collected in the dashboard, where certain quality indicators associated with delirium, including the patient’s length of stay, can be evaluated. Dr. Factora says the data can help clinicians evaluate the success of their efforts and avoid treatment decisions that could potentially worsen a patient’s symptoms.
The delirium dashboard can also help improve communication between nurses and physicians – an essential component of high-quality care, he explains. “It’s an efficient, transparent way to ensure that every member of the clinical team is on the same page. Not only does the dashboard inform caregivers that a problem is present, it also details the steps that have been taken to address it across the continuum of care,” notes Dr. Factora.
Advertisement
Nurses, who are typically charged with implementing clinical screening throughout the hospital, can administer a set of orders designed to help instruct doctors and other medical providers in the management of delirium. These guidelines include consults with specialists in geriatrics or psychiatry, he says.
Dr. Factora explains that one of his team’s chief goals is to use the dashboard to help improve documentation and communication – particularly during “transition” periods, when a patient is discharged from the hospital and transferred to a post-hospital setting. Without thorough reporting and clear communication, a patient’s delirium may be overlooked upon discharge and go untreated by subsequent caregivers. Such oversights can lead to serious problems, he says, including the discontinuation of medications prescribed in the hospital for high-risk delirium-related behaviors.
“These patients must be monitored carefully for cognitive decline, even after hospitalization; without appropriate care, their symptoms can worsen,” says Dr. Factora. “When we initiate a handoff to an outside facility, it is critical to communicate the patient’s current delirium status and any treatments they received while in our care. Continuity is a valuable part of any medical plan, but it’s imperative when managing patients with delirium – a disorder that can have grave consequences if not properly addressed.”
Looking to the future, Dr. Factora and his colleagues are working to build a core team to assist in the prioritization of delirium recognition and documentation. “I hope our work can also help improve the ability of our outpatient doctors to recognize delirium and follow their patients longitudinally to ensure that they recover as well as they possibly can.”
Advertisement
Advertisement

Researchers explore the mental and physical benefits of social prescribing

Multidisciplinary approach helps address clinical and psychosocial challenges in geriatric care

Effective screening, advanced treatments can help preserve quality of life

Study suggests inconsistencies in the emergency department evaluation of geriatric patients

Auditory hallucinations lead to unusual diagnosis

How providers can help prevent and address this under-reported form of abuse

How providers can help older adults protect their assets and personal agency

Recognizing the subtle but destructive signs of psychological abuse in geriatric patients