Guidelines for treatment, screening and genetic testing
With so much ground to cover in a well-child visit, cholesterol may not be at the top of your mind. After all, cardiovascular disease doesn’t usually develop until after age 55 in men and age 65 in women. However, many young patients have elevated LDL cholesterol levels caused by familial hypercholesterolemia (FH). If proper screening measures aren’t taken, the health of the patient and their entire family could be in jeopardy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
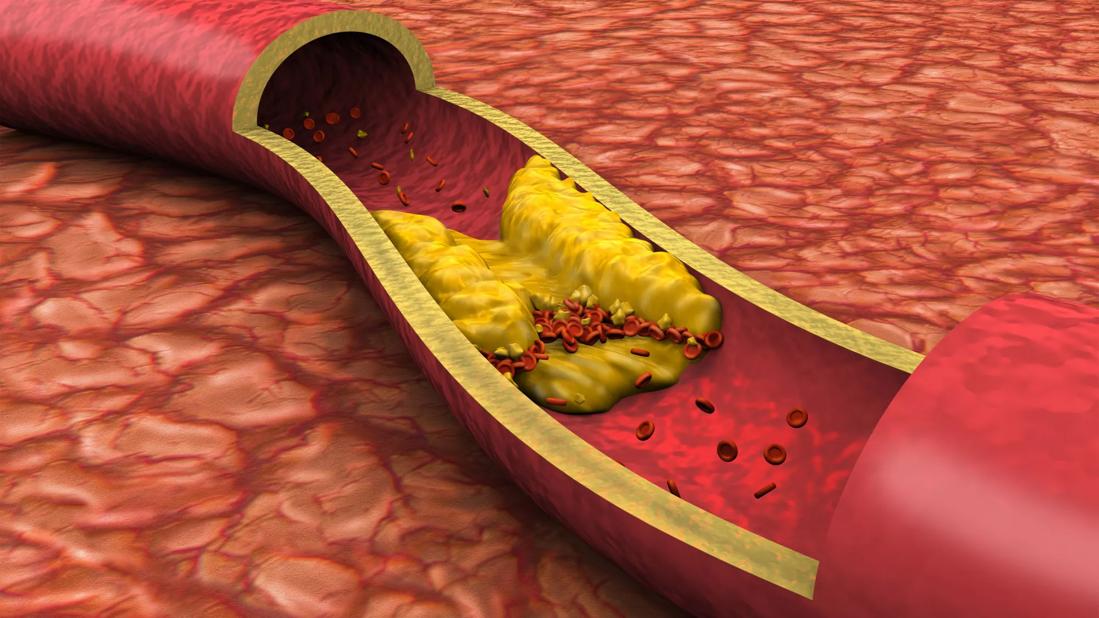
FH is an inherited disorder caused by an abnormal mutation of one or more of the genes responsible for cholesterol metabolism. Instead of processing LDL in the liver properly, the body has increased deposits in the blood vessels causing cholesterol plaques. Patients with a long history of elevated LDL can begin developing significant atherosclerotic cardiovascular disease (ASCVD) as early as age 30 in men and age 40 in women.
“In addition to elevated LDL levels, patients with FH also tend to have low HDL levels,” explains Christina Fink, MD, pediatric cardiologist and head of the Lipid Clinic at Cleveland Clinic Children’s. “A first-degree relative with high LDL is also a probable indicator of FH. However, young patients may not have a family history of high LDL, especially if the gene mutation for FH starts with the child.”
According to the Journal of the American Heart Association, FH affects about 1 in 220 individuals in the U.S. It can be diagnosed as early as the first few years of a patient’s life.
The Journal of Pediatrics recently published the results of a study that analyzed the enrollment characteristics of young patients in a national FH registry. Key highlights of the study include:
Advertisement
“Collecting data for FH patients provides useful baseline data to help recognize disease characteristics and explore patient profiles,” notes Dr. Fink. “This study also highlights the importance of screening to facilitate early intervention in order to prevent negative outcomes.”
When it comes to managing high cholesterol, lifestyle plays an important role. “When we have patients with LDL levels around 190, we start by analyzing their diet and exercise history as well as their screen habits,” explains Dr. Fink. “We typically give them three to six months to improve to see if they can get their LDL levels below 160 naturally.”
“Young patients who are willing to make changes might be able to lower their LDL by 20%, which could postpone treatment for several years as we continue to monitor their condition,” Dr. Fink reveals. “But if you have FH, lifestyle changes typically will not be enough to get you to the recommended threshold for your age group. Plus, LDL levels tend to creep up over time and eventually require medication.”
Statins are the most common form of lipid-lowering treatment and have been shown to be fairly safe and well-tolerated in children. “We can treat children with FH as early as age 8, when the LDL concentration is greater than 250. But we typically wait until age 10,” says Dr. Fink. “It’s important for family members to comply with medication recommendations and overcome any stigma they may have about statins.”
FH is diagnosed with a simple blood test. In harmony with the national guidelines, Dr. Fink recommends the following best practices for screening at well-child visits:
Advertisement
“If we screen children at age 9 versus age 2, we’ll still catch the LDL problem,” explains Dr. Fink. “But if we can identify these children sooner, we can do cascade screening for the whole family and potentially save multiple people from premature ASCVD.”
“Even if a child looks otherwise healthy, it’s important to ask parents about their own health issues during well-child visits and investigate them promptly,” Dr. Fink emphasizes.
If genetic testing is desired, Dr. Fink recommends consulting a genetic specialist as well as a genetic counselor. The counselor can help interpret test results and recommend next steps. “While it can be helpful to identify the specific genetic cause of FH, the most important thing you can do is biochemically screen your family members for high LDL levels,” she says.
If your patient has an LDL greater than 190, refer the patient to a lipid specialist. If your patient has an LDL around 160 or 170, it may be helpful to refer the patient to a specialist when diet and exercise are unable to bring levels down to less than 130.
Advertisement
Advertisement

Findings hold lessons for future pandemics

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes