A screening blood test would be a huge step toward earlier intervention
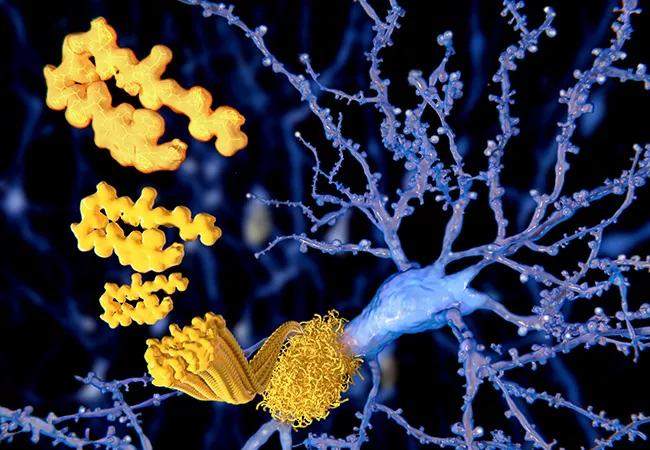
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/881f85f9-31d0-4322-a8f4-db36b0877268/20-NEU-2024366_alzheimer-brain-pathology_650x450_jpg)
20-NEU-2024366_alzheimer-brain-pathology_650x450
By Lynn M. Bekris, PhD, and James B. Leverenz, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This article is reprinted from Cleveland Clinic Journal of Medicine (2020;87[9]:537-539).
Emerging blood-based biomarkers for Alzheimer disease are an exciting new development in the dementia field, since they may offer a broadly accessible and relatively inexpensive screening tool. Looking to the future, when disease-modifying or prevention treatments will be available, investigators are focused on how to detect the earliest biological signals of Alzheimer disease, perhaps even years or decades before clinical symptoms appear.
The current standard workup for a patient with dementia symptoms focuses on disorders that may look like dementia or aggravate the early symptoms of Alzheimer disease or a related dementia (e.g., metabolic disorder, structural abnormality, vitamin deficiency). Currently, patients and their families want to know, Is this Alzheimer disease, or something that can be reversed? Current diagnostic testing can be challenging due to complexity, cost or level of intervention. A validated blood test that could be widely utilized would be big step forward for diagnosing and, hopefully, intervening before a patient becomes clinically impaired.
An astonishing 5.8 million Americans age 65 and older have Alzheimer disease or a related dementia, and this number is expected to increase to 13.8 million by 2050.1
The impact on families is both financial and emotional. More than 16 million Americans currently provide unpaid care for family members or friends with dementia. The projected national cost of caring for those with Alzheimer disease and other dementias is currently $305 billion. As the aging population increases, so does the population with Alzheimer disease. The burden of caring for the increasing aging population with dementia is exacerbated by a shortage of dementia care specialists and the increasing burden on primary care clinicians to identify and provide care for these patients.1
Advertisement
The pathologic hallmarks of Alzheimer disease are the accumulation in the brain of extracellular amyloid beta plaques and intra-neuronal inclusions (neurofibrillary tangles) consisting of phosphorylated tau, a microtubule-associated protein. Other features are dystrophic neurites, loss of synapses, neuronal death and gliosis. These pathologic changes can begin 10 to 20 years before the onset of clinical symptoms.2
Current validated biomarkers of Alzheimer disease pathology include:
The memory specialist is faced with a multitude of nuanced and mixed pathologies underlying a dementia syndrome.5 Biomarkers of Alzheimer disease pathology in combination with cognitive assessment and structural brain imaging can be valuable diagnostic tools in these circumstances. However, cerebrospinal fluid analysis and PET are not easily utilized by the primary care clinician due to access, comfort with the testing or interpretation, and expense. Furthermore, the bedside cognitive testing currently used by primary care providers does not easily identify patients with early cognitive changes.
Therefore, for the primary care clinician, less-invasive and less-specialized screening tools, such as a blood test, would be a significant development. These screening tools could help determine who should be referred for more in-depth testing. Recent developments in the field are bringing us closer to blood tests that primary care clinicians can use as screening tools. This trend is promising, since it also will help in developing therapies targeting early-stage Alzheimer disease-specific pathology in larger and wider populations. Blood testing could fit into a diagnostic algorithm — similar to testing for certain cancers — that the primary care clinician could use for those at high risk of Alzheimer disease, such as the elderly and those with a strong family history.
Advertisement
A major barrier to developing new drugs for Alzheimer disease is that it is hard to identify patients who are in the early stage of the disease, soon after the pathologic changes in the brain have begun but before cognitive impairment has become apparent, especially in the primary care setting. Given that an inexpensive and sensitive blood-based biomarker would enhance the ability of the primary care clinician to screen for possible Alzheimer disease, many researchers have focused significant effort on developing one.
Circulating amyloid beta. In early studies, plasma levels of amyloid beta lacked a consistent association with Alzheimer disease.6 This was most likely due to assay-related difficulties, since plasma measurements of this protein may be influenced by matrix effects whereby other proteins in plasma bind it. However, later studies using more sensitive assays indicated that the plasma ratio of the amyloid beta 1–42 and 1–40 peptides was lower in amyloid PET-positive individuals, as it is in the cerebrospinal fluid,7-11 strongly suggesting that a plasma 1–42-to-1–40 ratio may be a feasible blood-based biomarker of Alzheimer disease. The only missing piece was a blood-based measure of tau.
Plasma total tau. Initial studies of blood-based tau suggested that the plasma total tau concentration is higher in patients with Alzheimer disease than in cognitively normal controls. Unfortunately, the difference was not as clear or as well replicated as in cerebrospinal fluid.6 Subsequent studies also reported elevated plasma total tau in Alzheimer disease12,13 and an association with faster clinical disease progression,12 supporting the idea that plasma tau is indeed significantly elevated in Alzheimer disease.
Advertisement
Plasma phosphorylated tau 181, tau 217. Since cerebrospinal fluid phosphorylated tau 181, a key component of neurofibrillary tangles, adds better diagnostic accuracy than tau alone, researchers developed a new assay for phosphorylated tau at amino acid 181 in plasma. An association between this new phosphorylated tau 181 test and amyloid beta, as well as tau PET, was even stronger than those obtained using the plasma total tau test,14-16 providing strong evidence that plasma-phosphorylated tau 181 is a feasible blood-based biomarker of Alzheimer disease. However, since tau is phosphorylated at many sites, other phosphorylated sites may be better circulating biomarkers of Alzheimer disease. Most recently, intriguing new findings suggest that the plasma tau phosphorylated at amino acid 217 differs in patients with Alzheimer disease compared with cognitively normal controls and people with other neurodegenerative disorders.17,18 Plasma phosphorylated tau 217 is an intriguing finding, since it appears to outperform plasma phosphorylated tau 181 and imaging markers in terms of diagnostic accuracy.17,18
While these new findings are encouraging, they are early results. These blood-based tests need further testing in large-scale studies over the long term to refine and verify them, especially in the general population.
There is as yet no gold-standard biomarker for Alzheimer disease (or for vascular dementia) before clinical symptoms arise. Definitive diagnosis is done at autopsy, based on neuropathologic amyloid and tau findings.
Advertisement
The Alzheimer’s Association Global Biomarker Standardization Consortium (GBSC) was established more than a decade ago to bring together key researchers, clinicians, industry, regulatory bodies and government leaders in Alzheimer disease and other dementias.19 The goal is to achieve consensus on the best way to standardize and validate biomarker tests for use in clinical practice. Promising biomarkers have spurred several method-comparison and standardization studies across multiple laboratory sites, both nationally and internationally, under GBSC guidance. Future method-comparison and standardization studies will bring us closer to plasma amyloid and tau biomarkers as effective screening tools in the primary care setting.
This is an exciting time, since blood-based biomarkers for Alzheimer disease are a potentially important step forward for both research and clinical care. As we move toward disease-modifying therapies for Alzheimer disease and related dementias, they will be crucial for enhancing further clinical trial strategies, supporting primary care practice diagnosis and management and, hopefully, moving to an era of better interventions for these devastating disorders.
Dr. Bekris is associate staff in Cleveland Clinic’s Genomic Medicine Institute and Lerner Research Institute. Dr. Leverenz is Director, Cleveland Clinic Lou Ruvo Center for Brain Health, Cleveland.
Advertisement
Initiatives focus on the physical and emotional well-being of geriatric patients and their caregivers
Researchers explore the mental and physical benefits of social prescribing
Multidisciplinary approach helps address clinical and psychosocial challenges in geriatric care
Effective screening, advanced treatments can help preserve quality of life
Study suggests inconsistencies in the emergency department evaluation of geriatric patients
Auditory hallucinations lead to unusual diagnosis
How providers can help prevent and address this under-reported form of abuse
How providers can help older adults protect their assets and personal agency