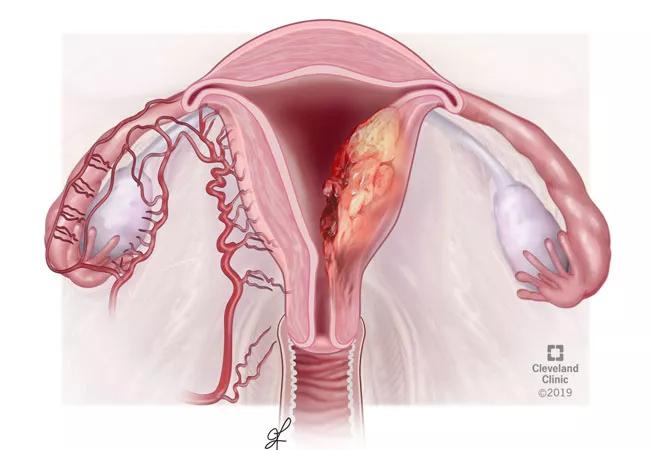
Characterizing endometrial cancer in young patients diagnosed before age 40
by Ji Son, MD, MS, Mariam AlHilli, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The prevalence of endometrial cancer in women 40 years and younger has been previously estimated at approximately 5%. Due to the rarity of this diagnosis in young women, few studies exist examining the clinical characteristics of young women with endometrial cancer. At the Society for Gynecologic Oncology’s 50th Annual Meeting on Women’s Cancer, held in Honolulu from March 16-19, 2019, we presented data characterizing endometrial cancer in patients diagnosed before age 40 who received cancer care at Cleveland Clinic.
The diagnosis of endometrial cancer in young women can be difficult to make, compared to older and postmenopausal women who present with postmenopausal bleeding. Age is an important prognostic factor in endometrial cancer, as increased age is associated with worse survival and a higher risk of recurrence. Research is limited regarding survival in endometrial cancer in younger women. In addition, many young women with endometrial cancer may desire fertility-preservation, in which they choose to undergo non-surgical treatment with anti-estrogen medication or intrauterine device to maintain their ability to get pregnant in the future. The impact of this strategy on endometrial cancer outcomes is unknown. To our knowledge, this is one of the largest groups of patients under age 40 with endometrial cancer studied in the literature to date.
We found that young women with endometrial cancer are more likely to be obese and harbor a concurrent ovarian cancer. The rate of concurrent ovarian cancer in our population was approximately 9%. Having a diagnosis of ovarian cancer at the same time as endometrial cancer does not seem to affect a patient’s prognosis since both cancers are typically diagnosed at an early stage. One in five women in our cohort of patients chose to preserve fertility. However, this strategy was successful in less than 25% of these patients.
Advertisement
Our data confirm previous findings that younger women with endometrial cancer have more favorable prognostic factors compared to older patients. In our analysis, we found that women under 40 with endometrial cancer are more likely to recur than patients with endometrial cancer in the 41-60 age group after adjusting for known adverse prognostic factors. Although this may be due to failure of medical therapy, this treatment strategy does not adversely affect overall survival as most of these patients eventually undergo definitive surgical treatment. The success of this treatment strategy requires close surveillance by a gynecologic oncologist and the involvement of a multidisciplinary care team.
Women in our study underwent screening for Lynch syndrome through a pathology-based test. Based on this, women were classified to have intact mismatch repair protein expression or deficiency (also known as microsatellite instability). Women with Lynch syndrome are often diagnosed with endometrial cancer at a younger age. However, we found that the incidence of Lynch syndrome and mismatch repair deficiency was not influenced by age, and that mismatch repair deficiency predicted a worse prognosis when caused by methylation of the gene MLH1. There is ongoing research on the use of mismatch repair protein deficiency as a prognostic marker in endometrial cancer, which will be critical in the contemporary management of endometrial cancer.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors