Multicenter observational study shows no simple answer
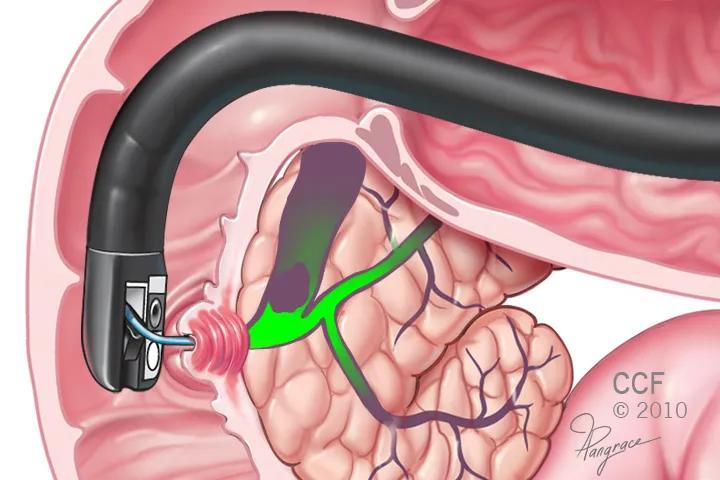
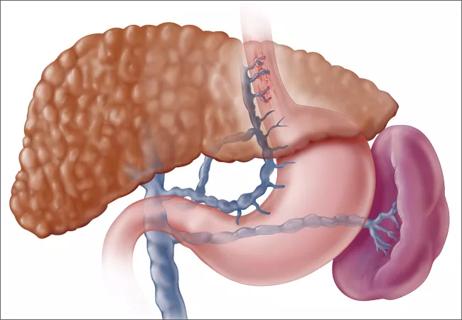
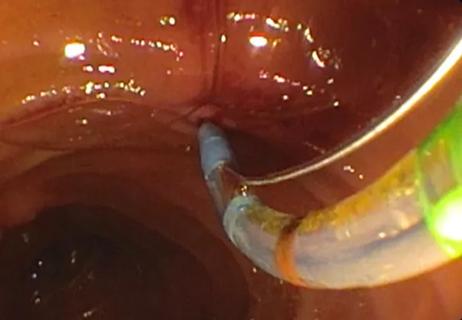
Research has shown that general anesthesia with intubation is associated with higher risk of hypotension, while utilizing anesthesia without intubation is associated with an increased risk of hypoxemia. However, it has long been unclear which is a better option for patients undergoing complex procedures like endoscopic retrograde cholangiopancreatography (ERCP). Now, a study presented at Digestive Disease Week 2021 shows that neither approach is a clear winner.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“It was a photo finish,” says John J. Vargo, MD, MPH, gastroenterologist and Enterprise Endoscopy Director at Cleveland Clinic’s Digestive Disease & Surgery Institute, and coauthor of the study. “Each approach held its own advantage as well as a disadvantage.”
The findings, he said, indicate that anesthesiologists should customize their approach to the risk factors of the individual patient.
While the specific results were not a surprise, the size of the study should definitively lay to rest the question of whether one option is superior, Dr. Vargo says. The researchers also looked at cases in which the patient was converted from sedation to general anesthesia during the procedure and identified associated risk factors.
The observational study analyzed case data from the Multicenter Perioperative Outcomes Group in more than 61,000 non-emergent ERCP patients from 2006 to 2019. Patients who received general anesthesia with intubation had 1.27 times higher odds of experiencing low blood pressure, while those who underwent sedation without planned intubation had 1.51 times higher odds of low oxygen levels. Case and anesthesia duration was slightly longer in the general anesthesia group compared with the sedation group, with a median of 57 and 81 minutes, compared with 48 and 69 minutes.
“There’s not a cookie cutter approach to who should get intubated,” Dr. Vargo says. “So, for someone with a penchant for hypotension, maybe you want to consider without intubation. If you have a patient who has a penchant for hypoxemia, maybe that patient should be intubated.”
Advertisement
The study also found that 6.5% of sedation cases were converted to general anesthesia during the procedure. Risk factors for conversion included liver disease and race, as well as procedure room type and higher institutional procedure volume.
Patients in operating rooms (OR) were more likely to be converted to general anesthesia than those in an endoscopy procedure room, perhaps related to the physician’s comfort and ease of working in a dedicated procedure room, or because patients with advanced comorbidities were more likely to be treated in an OR. Similarly, higher-volume facilities likely receive more complex or acute cases, Dr. Vargo notes.
The key takeaway is for providers to consider all risk factors in choosing the best anesthesia option for ERCP. “For example, in a patient with severe liver disease, you may want to think about how the conversion rate was higher for those patients,” he says. “There’s no right or wrong answer, it’s just doing the right thing for the patient.”
Advertisement
Advertisement

Although the number of surgeon-scientists in colorectal surgery is small, a Cleveland Clinic colorectal surgeon-scientist shares his thoughts on what surgeon-scientists bring to the table

The unique program addresses an unmet need and continues to expand

A three-step plan aimed at strengthening the institute’s infrastructure includes a renewed focus on mentorship

Expert panel endorses greater access based on research showing procedures’ safety and efficacy

First two cases set the course for a full spectrum of intrauterine therapies
Providers must inform patients of guarded prognosis

A discussion of why it's time to start treating obesity differently
Patients can go home the same day