Expert panel endorses greater access based on research showing procedures’ safety and efficacy
An international panel of experts has issued new evidence-based guidelines that call for dramatically expanding patients’ eligibility for metabolic and bariatric surgery (MBS), including recommending that children and adolescents with obesity be considered for weight-loss surgery under certain conditions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The report, prepared on behalf of the American Society for Metabolic and Bariatric Surgery and the International Federation for the Surgery of Obesity and Metabolic Disorders, two of the world’s leading authorities on MBS, advocates significantly lowering the body mass index (BMI) threshold at which surgery should be considered.
The new guidance replaces more restrictive criteria for weight-loss surgery in place for three decades. It reflects a wealth of research in recent years confirming MBS’ safety and long-term effectiveness in treating severe obesity and its comorbidities.
The recommendations also are driven by the urgent need to stem the rapidly increasing prevalence of obesity — a chronic, complex, multifactorial disease that afflicts 13% of the world’s population, causing millions of deaths and billions of dollars of healthcare expenditures annually.
“The field of metabolic and bariatric surgery has progressed considerably in the last 20 years,” says Ali Aminian, MD, Director of Cleveland Clinic’s Bariatric & Metabolic Institute and a member of the panel that developed the new criteria. “I hope these guidelines can open the doors for some patients who did not have access to bariatric and metabolic surgery by the old guidelines, which were outdated. And I hope that healthcare providers and insurance providers become familiar with these new guidelines and understand that there are safe and effective treatments for obesity available.”
The panel’s recommendations, though not compulsory, are meant to serve as standards for clinicians and patients when making decisions about whether and when MBS should be utilized. The advisory also could influence insurers’ decisions on whether and when to cover the procedures’ cost.
Advertisement
The MBS guidelines currently in use were issued in 1991 by a National Institutes of Health (NIH) consensus group. Hundreds of studies examining worldwide experience with MBS have been published in the interim, including Cleveland Clinic-led research showing that the procedures can improve and reverse type 2 diabetes, lower the risk of developing obesity-related cancers, decrease risk of progression of fatty liver disease to cirrhosis, confer significant protective effects for future heart attacks or strokes, and lessen the severity of COVID-19 infection.
“We at Cleveland Clinic are one of the most productive bariatric surgery centers in the world in terms of conducting high-quality research and providing practice-changing data,” Dr. Aminian says. “Many of the studies cited in the new MBS guidelines came from our work.”
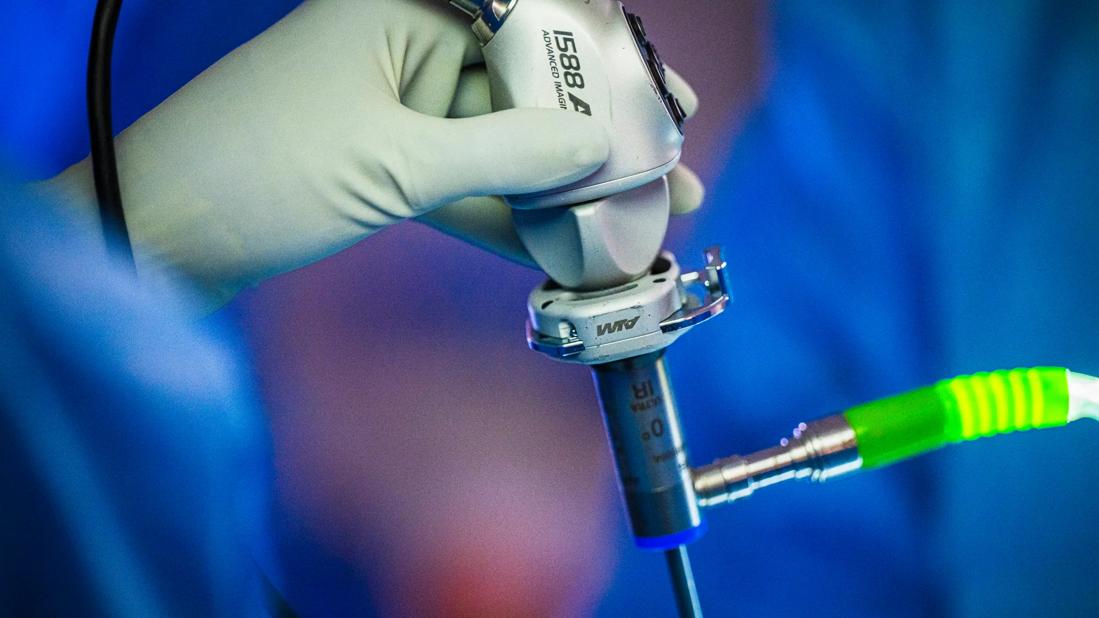
Collectively, research shows that MBS consistently produces superior, durable weight-loss outcomes compared with medical treatments for obesity, with very low operative mortality rates (0.03%-0.2%). Older procedures such as adjustable gastric banding and vertical banded gastroplasty have been supplanted or become subordinate to more effective approaches. Many formerly open MBS procedures are now performed laparoscopically, resulting in fewer complications, reduced hospital stays and decreased risk of surgical site infections and postoperative abdominal wall hernias. Two laparoscopic procedures — Roux-en-Y Gastric Bypass and sleeve gastrectomy — now account for about 90% of all weight-loss surgeries performed worldwide.
Advertisement
“At the time the first MBS guidelines were issued, the risk of dying from the surgery was about two or three percent; now it is about one out of 1,000,” Dr. Aminian says. “All of the procedures were open surgeries and patients used to require hospital stays of five to seven days and took months to recover. Many patients developed hernias at the incision site, of which almost half required a second operation for hernia repair. Now we do surgery through five or six small holes, patients go home the same day or the next day, and they recover after two or three days. We have procedures that are much safer and produce better metabolic effects. Patients who undergo bariatric surgery typically lose 20% to 40% of their body weight and sustain it over decades. In recent years, Cleveland Clinic’s bariatric surgery program has had zero mortality and no gastrointestinal leaks.”
Despite those advances and benefits, MBS utilization rates remain extremely low. That may be due in part to the 1991 consensus document’s conservative approach to surgical eligibility. Those guidelines set the universal threshold for MBS surgery at a BMI ≥40 kilogram/meter2 (class 3 or severe obesity), or ≥35kg/m2 for patients with obesity-related comorbidities such as heart disease and hypertension.
The new standards significantly lower the eligibility threshold, strongly recommending MBS for patients with a BMI ≥35 kg/m2 (class 2 obesity), regardless of whether comorbidities are present. The guidance also strongly recommends MBS for patients with BMI ≥30kg/m2 and type 2 diabetes. In patients with class 1 obesity (BMI 30-34.9 kg/m2), the panel says MBS should be considered if an initial trial of nonsurgical therapy is unsuccessful in achieving substantial, durable weight loss and resolving comorbidities such as hypertension, cardiovascular disease, chronic kidney disease or fatty liver disease.
Advertisement
The guidelines say children and adolescents with a BMI >140% of the 95th percentile (class 3 obesity), and those with a BMI >120% of the 95th percentile (class 2 obesity) and a major comorbidity, should be considered for MBS after evaluation by a multidisciplinary team in a specialty center.
The 1991 NIH consensus guidelines were silent on the issue of MBS for those under 18, even in cases where BMI exceeded 40 kg/m2, citing a lack of research to justify a recommendation. Subsequent studies have demonstrated the safety and efficacy of MBS in this age group, including durable weight loss and sustained reduction in comorbidities in children as young as 5.
“All of the data we for have for bariatric and metabolic surgery in adolescents shows the success rate in terms of controlling comorbid conditions of obesity is much better compared with outcomes in adults,” Dr. Aminian says. “If you have a 16-year-old with obesity and recently diagnosed diabetes and hypertension and we take care of those right away, the outcome is much better than the patient carrying those comorbidities for 10 years or more.”
The new guidelines do not endorse an upper age limit for MBS, noting that complication rates for patients older than 70 are slightly higher than in younger individuals but that the surgery still provides substantial benefits in terms of weight loss and comorbidity reduction. Factors such as frailty and cognitive status probably have a greater impact than age on the procedures’ efficacy and complication rates in older patients, the report says.
Advertisement
“At Cleveland Clinic, we operate in patients in their 70s and 80s if they are physiologically fit and can tolerate the surgery,” Dr. Aminian says.
Patients with a BMI exceeding 60 kg/m2 require special consideration to safely undergo MBS due to potential surgical and mortality risks, but the expert panel concludes that carefully selected individuals with extreme BMI should be eligible.
Earlier intervention is preferable, however, Dr. Aminian stresses.
“Obesity is a progressive disease and it is always safer to intervene earlier in its course, while a patient has class 1 or 2 obesity, rather than waiting until patient gains more weight and develops a more severe form of disease,” he says. “For patients with heart disease, we don’t wait to treat until they experience a heart attack. For patients with cancer, it is always better to start treatment in the earliest stage. A similar concept is true when we consider weight-loss surgery to treat obesity. Surgery shouldn’t be viewed as the last resort, only for patients with extremely high BMI.”
Dr. Aminian and his colleagues on the expert panel acknowledge that BMI is an imperfect proxy for obesity. It does not reflect obesity’s metabolic burden and is only an approximation of adiposity that does not take into account relevant factors such as a person’s sex, age and ethnicity, and whether body fat has accumulated subcutaneously or viscerally — the latter associated with metabolic and cardiovascular disease.
“We had long discussions about creating guidelines based on something new or innovative, away from BMI,” Dr. Aminian says. “But we wanted to have guidelines that can be used everywhere, and measuring the body composition is not available universally, which may cause challenges for patients who already have limited access to surgery. So we decided to continue with BMI, although we know it has limitations.”
Recognizing that BMI criteria do not apply equally to all populations, the guidelines establish a lower BMI threshold for MBS eligibility in Asian patients, since the prevalence of diabetes and cardiovascular disease in the Asian population is higher at a lower BMI compared with non-Asian populations. The expert panel determined that a BMI ≥25 kg/m2 in Asian people is indicative of clinical obesity, and that MBS is recommended for Asian individuals with a BMI ≥27.5 kg/m2.
Robust data do not currently exist to allow similar correlation between lower BMI levels and risk of cardiometabolic disease in other ethnic or racial groups. Additional research may help fill that void.
“There are a lot of unknowns about the pathogenesis and course of obesity and metabolic disease,” Dr. Aminian says. “In the future, it is likely that we will have a better understanding of the disease process, which will allow us to take a more individualized approach to treatment. But for now, treating our patients based on certain BMI thresholds is the most practical way to address obesity.”
The new MBS guidelines come at a time when the global pandemic of obesity is worsening. In the United States, the prevalence of obesity increased from 30.5% to 41.9% between 2000 and 2017 and is projected to reach 50% by 2030, with one in four cases constituting severe (class 3) obesity.
“Every single country has miserably failed in controlling obesity in the past three decades and it continues to get worse,” Dr. Aminian says. “That’s because we only emphasize lifestyle modification. Obesity is a chronic progressive disease and it really requires aggressive treatment.”
While MBS is effective, only 1% of patients eligible for weight-loss surgery under the previous guidelines actually underwent the procedures, he says. The reasons range from patients and healthcare providers not knowing the operations’ safety and efficacy to patients’ lack of insurance coverage and insurers’ unwillingness to routinely and comprehensively reimburse for the cost of MBS.
The new guidelines should help in addressing some of those issues, Dr. Aminian says — particularly in making the case for expanded insurance coverage, which is essential in order to increase patients’ access to MBS.
“The field has progressed significantly, but unfortunately the guidelines had not been updated for a long period of time,” he says. “At least now we have the latest information compiled in one document. It’s up to us to reach out to insurance companies and communicate with them about the guidelines and supporting data. We have numerous analyses that show metabolic and bariatric surgery is cost-effective in the long run because of the reduction or elimination of comorbidities and the associated cost of medications needed to treat them. I’m not one hundred percent certain that everything will change with these new guidelines, but it’s a good start.”
Advertisement

Researchers explore how changes in the gut microbiome influence the brain's reward response to alcohol

Surgical intervention linked to increased lifespan and reduced complications

Retrospective study highlights psychosocial predictors of bariatric surgery outcomes

Comprehensive mental health screening may help prevent postsurgical risks

Consider each patient's unique disease progression and treatment goals when choosing a strategy

Sustained weight loss helps reduce IIH symptoms and medication dependence

Findings could help identify patients at risk for poor outcomes

Findings show greater reduction in CKD progression, kidney failure than GLP-1RAs